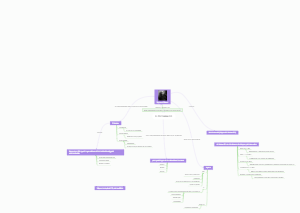
MindMap Gallery Classification of Psychopathology
- 14
Classification of Psychopathology
This mind map provides a comprehensive classification of psychopathology, detailing various categories of mental disorders. It starts with the main topic "Classification of Psychopathology" and branches out into major categories such as Neurocognitive Disorders, Mood Disorders, Psychotic Disorders, Anxiety Disorders, and more. Each category is further subdivided into specific disorders, with some including additional characteristics or criteria. For example, Substance Use Disorder lists Dx Criteria including tolerance, withdrawal, and social occupational decline. This visual representation helps in understanding the complex structure and relationships within psychopathology classifications.
Edited at 2025-10-06 02:54:37- Psychopharmacology Mind Map
This detailed mind map, created using EdrawMind, provides a comprehensive overview of psychopharmacology, focusing on pharmacological treatments for psychotic symptoms. It branches into key categories including antipsychotics (both typical and atypical), antidepressants, anti-epileptic medications (AEDs) used in mood stabilization and anti-seizure treatments, and their applications in specific populations and conditions such as Parkinson's disease psychosis and lactating mothers with bipolar disorder, offering a structured insight into the field.
- Classification of Psychopathology
This mind map provides a comprehensive classification of psychopathology, detailing various categories of mental disorders. It starts with the main topic "Classification of Psychopathology" and branches out into major categories such as Neurocognitive Disorders, Mood Disorders, Psychotic Disorders, Anxiety Disorders, and more. Each category is further subdivided into specific disorders, with some including additional characteristics or criteria. For example, Substance Use Disorder lists Dx Criteria including tolerance, withdrawal, and social occupational decline. This visual representation helps in understanding the complex structure and relationships within psychopathology classifications.
- Depressive Disorders Diagnosis and Assessment
This mind map provides a comprehensive overview of depressive disorders, focusing on diagnosis and assessment. It covers medications associated with depression, drugs of abuse that can induce depression, and secondary depression medical etiologies. The map details specific medical conditions that can lead to depression, such as neoplasms, immune disorders, cardiac conditions, endocrine disorders, and neurologic disorders. Additionally, it outlines the diagnosis criteria for substance/medication-induced depressive disorder and depression due to another medical condition, highlighting core symptoms and contributing factors.
Classification of Psychopathology
- Psychopharmacology Mind Map
This detailed mind map, created using EdrawMind, provides a comprehensive overview of psychopharmacology, focusing on pharmacological treatments for psychotic symptoms. It branches into key categories including antipsychotics (both typical and atypical), antidepressants, anti-epileptic medications (AEDs) used in mood stabilization and anti-seizure treatments, and their applications in specific populations and conditions such as Parkinson's disease psychosis and lactating mothers with bipolar disorder, offering a structured insight into the field.
- Classification of Psychopathology
This mind map provides a comprehensive classification of psychopathology, detailing various categories of mental disorders. It starts with the main topic "Classification of Psychopathology" and branches out into major categories such as Neurocognitive Disorders, Mood Disorders, Psychotic Disorders, Anxiety Disorders, and more. Each category is further subdivided into specific disorders, with some including additional characteristics or criteria. For example, Substance Use Disorder lists Dx Criteria including tolerance, withdrawal, and social occupational decline. This visual representation helps in understanding the complex structure and relationships within psychopathology classifications.
- Depressive Disorders Diagnosis and Assessment
This mind map provides a comprehensive overview of depressive disorders, focusing on diagnosis and assessment. It covers medications associated with depression, drugs of abuse that can induce depression, and secondary depression medical etiologies. The map details specific medical conditions that can lead to depression, such as neoplasms, immune disorders, cardiac conditions, endocrine disorders, and neurologic disorders. Additionally, it outlines the diagnosis criteria for substance/medication-induced depressive disorder and depression due to another medical condition, highlighting core symptoms and contributing factors.
- Recommended to you
- Outline
Classification of Psychopathology
Neurocognitive Disorders NCDs
General Diagnostic Criteria 🧠
Exclusions Not exclusively during delirium, not better explained by another mental disorder
Level of Diagnostic Certainty & Specifiers
Certainty "Probable" or "Possible" regarding etiology, with specific criteria for each
Specifiers
With or without behavioral disturbance eg, psychotic symptoms, mood disturbance, agitation
Severity Mild, Moderate, Severe applies to Major NCD only
Severity
Major NCD Significant cognitive decline in ≥1 domain, interferes with independence in daily activities
MCQ Point The primary discriminator between Major and Mild NCD is interference with independence in daily activities
Mild NCD Modest cognitive decline, does not interfere with independence, but may require compensatory strategies
Classification by Etiology 🌍
Neurodegenerative
Alzheimer's Disease
AD Most common cause 66% Cortical deficits 4As amnesia, aphasia, agnosia, apraxia Often presents with memory and learning decline
Lewy Body Disease LBD
Second most common 20% Key features fluctuating cognition, recurrent detailed visual hallucinations, Parkinson motor symptoms starting after cognitive decline MCQ Point Severe neuroleptic sensitivity is a suggestive feature therefore antipsychotics should be avoided if possible
Vascular NCD
Third most common 15% Onset temporally related to cerebrovascular events Prominent decline in complex attention and frontalexecutive function Often has a stepwise progression Emotional incontinence pseudobulbar affect is common Control of vascular risk factors can improve cognition
Frontotemporal Lobar Degeneration FTLD
Often presents with disinhibition, apathy, dysexecutive syndrome, aphasia
Prion Disease eg, CreutzfeldtJakob Disease
CJD Insidious onset and rapid progression Motor features myoclonus, ataxia MCQ Point Fast polyphasic waves on EEG and CSF 1433 protein assay are supportive Always fatal, no accepted treatment
Huntington's Disease Neurologic
Traumatic Brain Injury TBI NCD
presents immediately after TBI or once consciousness recovered, then persists
Infectious
Neurosyphilis
HIV
Metabolic (Reversible causes)
eg, Vitamin B12 deficiency
Thyroid disease
Hepatic encephalopathy
Thyroid disease
Neoplastic (reversible causes)
eg, meningioma MCQ Point Neoplasms are reversible causes and a key ruleout for structural neuroimaging
Normal Pressure Hydrocephalus NPH Reversible cause of NCD
Mood disorder
Depressive disorder
Major Depressive Disorder MDD 😞
Criteria ≥5 symptoms present nearly every day for 2week period, with at least depressed mood or anhedonia
Specifiers
With Melancholic Features Loss of pleasure in all/almost all activities, lack of reactivity to pleasurable stimuli
With Atypical Features Mood reactivity is key Also, ≥2 of hypersomnia, increased appetite/weight gain, leaden paralysis, sensitivity to interpersonal rejection MCQ Point Classically responds to MAOIs
With Psychotic Features Delusions or hallucinations are present Can be moodcongruent themes of guilt, deserved punishment or moodincongruent persecutory, grandiose Treatment Antidepressant + Antipsychotic or ECT
With Catatonia ≥3 catatonic symptoms eg, stupor, catalepsy, mutism, waxy flexibility, echolalia, echopraxia
With Peripartum Onset Onset during pregnancy or within 4 weeks postpartum
With Anxious Distress
With Mixed Features
Comorbidities Very high lifetime comorbidity 72% with any other mental disorder Most frequent in pediatric depression Anxiety GAD, Panic, Disruptive Behavior Disorders ODD, CD, ADHD, Substance Use Disorders
Age of onset
Average Age of Onset: 29 years.
Late-Onset Depression: This is defined as the initial onset at 65 years or older.
Onset in Younger Populations:
Persistent Depressive Disorder Dysthymia
Disruptive Mood Dysregulation Disorder DMDD 🎭
Criteria Severe recurrent temper tantrums verbal/behavioral, disproportionate ≥3x/week Mood between tantrums persistently irritable/angry Present for ≥12 months in ≥2 settings MCQ Point Age of onset before 10 years Do not diagnose before age 6 or after age 18 Cannot be comorbid with ODD, Bipolar, or IED
Secondary Depressive Disorders
Due to Another Medical Condition Examples include AIDS, Lupus, Poststroke, Thyroid disease, Parkinson's, Huntington's, Alzheimer's, TBI, Obstructive Sleep Apnea
that is a direct pathophysiological consequence of another medical condition
vs Distinguish from
Adjustment Disorder: It's not just a psychological reaction to coping with a medical illness
Presence of atypical features of depression (e.g., unusual age of onset, absence of family history) can suggest a medical cause
Substance/MedicationInduced Due to prominent and persistent depressed mood or diminished interest/pleasure directly from substance/medication
Agent Capability
Alcohol: Most common legal depressant;
intoxication and withdrawal
Benzodiazepines
cause depressant effects; withdrawal can also induce depressive symptoms
Barbiturates: Known depressants
Hypnotics: Can lead to low mood; withdrawal can cause depression
Opioids/Opiates
Can cause depressive syndromes; withdrawal leads to dysphoric mood
Gammahydroxybutyrate (GHB)
Stimulants (mainly during withdrawal)
Amphetamines.
Nicotine (withdrawal)
Antihypertensive Agents
affecting catecholamine levels
Reserpine:
A classic MCQ culprit. It depletes monoamines (dopamine, norepinephrine, serotonin) and is a recognized cause of depression and suicide
Methyldopa
Clonidine
Hormonal agent
Corticosteroids / Steroids: Very commonly implicated in inducing depression (as well as euphoria, mania, or psychosis)
Oral Contraceptives
Thyroid Hormone (Dysregulation)
(e.g., hypothyroidism) can cause depressive symptoms
Antimicrobial
Isoniazid
Cephalosporins
Quinolones (e.g., Ciprofloxacin)
Temporal Relationship: Symptoms develop during or soon after substance intoxication, withdrawal, or medication exposure/change/withdrawal
Persistence:
If symptoms persist for a substantial period (e.g., about 1 month) after cessation of acute withdrawal or severe intoxication, it strongly suggests an independent depressive disorder rather than purely substance-induced. This distinction is frequently tested.
Bipolar disorder
Bipolar and Related Disorders
Overview of Bipolar Disorders
Definition and Characteristics
Distinct periods of abnormally elevated, expansive, or irritable mood and increased activity or energy 🌈
Bipolar I Disorder
Diagnostic Criteria
At least one manic episode required for diagnosis
Marked impairment in social or occupational functioning differentiates it from hypomania
Manic Episode Features
Distinct period of elevated mood for ≥1 week or any duration requiring hospitalization
Symptoms include grandiosity, decreased sleep, talkativeness, distractibility, and increased activity
Epidemiology and Prognosis
Average age of onset is 19 years significant suicide risk up to 50% attempt, 15% complete
Psychotic symptoms are common in 50% of cases
Bipolar II Disorder
Diagnostic Criteria
At least one hypomanic episode and one major depressive episode required
No manic episodes present
Features
Depression is more prominent than hypomania comparable suicide rates to Bipolar I
Rapid cycling is common, indicating frequent mood changes
Cyclothymic Disorder
Diagnostic Criteria
Numerous periods with hypomanic and depressive symptoms for ≥2 years ≥1 year for children/adolescents
Symptoms present at least half the time no major depressive, manic, or hypomanic episodes ever met 🌀
must never have been without symptoms for more than 2 months at a time
Age of onset: 15-25
Prevalence: 1% – M:F 1:1 in general population
Secondary Bipolar Disorders
Substance/MedicationInduced Bipolar Disorder
Mood disturbance directly from substance intoxication, withdrawal, or medication use
Medications like corticosteroids, antidepressants, and stimulants can induce mania
Dopamine agonists
L-DOPA
Sympathomimetics
Amphetamine
Cocaine
Pseudoephedrine
PCP
Antibiotics
◦ Ciprofloxacin
Clarithromycin
Anabolic and corticosteroids
Bipolar Disorder Due to Another Medical Condition
Direct pathophysiological consequence of a medical condition eg, CVA, seizure disorders
Differentiation from primary mania based on age of onset and related medical causes
Psychotic
Schizoaffective Disorder
Diagnostic Criteria
Major mood episode concurrent with schizophrenia criteria delusions or hallucinations present for 2+ weeks without mood episode
Prognosis
Better than schizophrenia but worse than mood disorders more psychotic symptoms predict poorer prognosis
Delusional Disorder
Diagnostic Criteria
Presence of one or more delusions for ≥1 month functioning not markedly impaired
presence of delusions without other prominent psychotic symptoms like hallucinations (if present, they are related to the delusion and not prominent), disorganized speech, or negative symptoms,
Patients generally maintain good functioning outside the direct impact of their delusion and their behavior is not overtly bizarre
Tends to be stable over time. Less than 25% progress to schizophrenia, and less than 10% develop a mood or bipolar disorder
Subtypes and Treatment
Subtypes include erotomanic, grandiose, and persecutory treatment includes antipsychotics
Patients often resistant to treatment but prognosis better than schizophrenia
Catatonia
Diagnosis and Symptoms
Requires ≥3 catatonic symptoms can be added to any mental disorder diagnosis
Treatment
Firstline treatment is Lorazepam avoid antipsychotics until catatonia resolves
ECT may be used for refractory cases
Schizophrenia
Diagnostic Criteria
At least two characteristic symptoms for ≥1 month delusions, hallucinations, or disorganized speech
Continuous signs of disturbance for at least 6 months
Positive and Negative Symptoms
Positive Delusions, hallucinations, disorganized behavior
Negative Diminished emotional expression, social withdrawal, lack of spontaneity
Epidemiology and Prognosis
Lifetime prevalence ~1% peak onset in males 1525 years and females 2535 years
Severity inversely related to age of onset negative symptoms predict poorer outcomes
Schizophreniform Disorder
Diagnostic Criteria
Symptoms same as schizophrenia for ≥1 month but less than 6 months
Prognostic Features
Good prognosis if symptoms appear within 4 weeks of behavior change and good premorbid functioning
Over 50% may progress to schizophrenia diagnosis
Brief Psychotic Disorder
Diagnostic Criteria
Positive symptoms for ≥1 day but less than 1 month with full return to premorbid functioning
Prognosis
4050% may progress to another psychotic illness, commonly schizophrenia
Psychotic Disorder Due to Another Medical Condition
Criteria
Prominent hallucinations or delusions as a direct consequence of a medical condition
Substance/MedicationInduced Psychotic Disorder
Criteria
Delusions or hallucinations during or soon after substance intoxication/withdrawal
Differentiation
Persistent symptoms suggest primary psychotic disorder if they last ~1 month postintoxication
Psychotic Disorders
Overview of Psychotic Disorders
Definition and Characteristics
Involve a break from reality, often with delusions or hallucinations 🌌
Other Specified/Unspecified Psychotic Disorder
Other Specified
Psychotic symptoms causing distress without meeting specific disorder criteria
Unspecified
Distress from psychotic symptoms without clear criteria for diagnosis
Anxiety disorders
Panic Disorder
Diagnostic Criteria
Characterized by recurrent unexpected panic attacks
Persistent concern about additional attacks or maladaptive behavioral changes
Key Features 🏃♂️
Approximately 30% experience nocturnal panic attacks
Sufferers often focus on interoceptive cues and catastrophize mild physical sensations
Risk factors include smoking and childhood abuse
Agoraphobia
Diagnostic Criteria
Marked fear or anxiety regarding at least two situations eg, public transport, open spaces, enclosed spaces, crowds, being outside home alone
Avoidance behavior or enduring situations with dread
Generalized Anxiety Disorder GAD
Diagnostic Criteria
Excessive anxiety and worry occurring more days than not for at least six months about various events or activities
Difficulty controlling the worry, with at least three associated symptoms restlessness, fatigue, concentration difficulty, irritability, muscle tension, sleep disturbance
Social Anxiety Disorder Social Phobia
Diagnostic Criteria
Marked fear or anxiety about one or more social situations where the individual may be scrutinized by others, fearing negative evaluation
Social situations are often avoided or endured with intense anxiety fear is disproportionate to the actual threat
Comorbidity Insights 📊
Commonly comorbid with avoidant personality disorder
Specific Phobia
Diagnostic Criteria
Marked fear or anxiety regarding a specific object or situation, provoking immediate fear/anxiety
The object/situation is actively avoided or endured with intense anxiety fear is out of proportion to actual danger, persisting for at least six months
Subtypes of Phobia 🐍
Animal
Natural environment
Bloodinjectioninjury
Situational
Other
Separation Anxiety Disorder
Diagnostic Criteria
Developmentally inappropriate and excessive fear or anxiety concerning separation from attachment figures
Adult Presentation Example
Can manifest in adults, such as a mother experiencing overwhelming anxiety about her schoolaged children
Anxiety Disorders
Overview of Anxiety Disorders
Definition and Characteristics
Defined by excessive fear and anxiety and related behavioral disturbances
Epidemiological Insights 🧠
High suicide risk associated with anxiety disorders
More prevalent in females compared to males
Chronic nature with episodes of waxing and waning
Neurotransmitter Involvement
Key neurotransmitters include norepinephrine, serotonin, GABA, and glutamate
Differential Diagnosis Ruleouts ⚠️
Medical Conditions
Cardiac issues eg, myocardial infarction, angina
Lung disorders eg, asthma
Endocrine disorders eg, pheochromocytoma, hyperthyroidism
Neoplasms eg, carcinoid syndrome
Neurological disorders eg, temporal lobe epilepsy, Huntington's disease
Electrolyte disturbances and B12 deficiency
Substance/MedicationInduced Conditions
Intoxication from stimulants, cocaine, hallucinogens, cannabis, nicotine, caffeine, and organophosphates
Withdrawal symptoms from alcohol, opiates, barbiturates, sedativehypnotics, SSRIs, and shortacting benzodiazepines like alprazolam
Neurodevelopmental Disorders Classification
General Principles
Definition of Neurodevelopmental Disorders
Conditions beginning early in development
Characterized by developmental deficits
Impairments in personal, social, academic, or occupational functioning
Classification of Specific Neurodevelopmental Disorders DSM5 Focus
Intellectual Disability ID / Intellectual Developmental Disorder
Key Diagnostic Criteria
Deficits in Intellectual Functions
Reasoning, problemsolving, planning, abstract thinking
Deficits in Adaptive Functioning
Failures to meet developmental and sociocultural standards
Primary measure of severity in DSM5
Onset During the Developmental Period
Identified during childhood or adolescence
Other Related Diagnoses
Global Developmental Delay
For children under 5 years with unreliable assessment
Unspecified Intellectual Disability
For individuals over 5 years with difficult assessment
Autism Spectrum Disorder ASD
DSM5 Changes
Combines previous Pervasive Developmental Disorders
Autistic Disorder, Asperger Syndrome, PDDNOS, etc
Reduced from three symptom categories to two core categories
SocialCommunication Impairment
Restricted, Repetitive Patterns of Behavior
Onset of symptoms in early developmental period
Specifiers
With or without intellectual impairment
With or without language impairment
Associated with known medical/genetic condition
Associated with another neurodevelopmental, mental, or behavioral disorder
With catatonia
Attention Deficit Hyperactivity Disorder ADHD
Presentation Types
Predominately Inattentive Presentation
Predominately Hyperactive/Impulsive Presentation
Combined Presentation
Severity Specifiers
Mild, Moderate, Severe
Can be specified as "in partial remission"
Tic Disorders
Tourette's Disorder
Requires both multiple motor tics and one or more vocal tics
Tics present for more than 1 year
Onset before age 18 years
Persistent Chronic Motor or Vocal Tic Disorder
Requires either motor or vocal tics
Tics present for more than 1 year
Onset before age 18 years
Provisional Tic Disorder
Requires single or multiple motor and/or vocal tics
Tics present for less than 1 year
Onset before age 18 years
Communication Disorders
Characterization
Persistent difficulties in language acquisition and use
Onset in the early developmental period
Types
Language Disorder
Difficulties in language acquisition and use
Phonological Disorder / Speech Sound Disorder
Difficulty with speech sound production
Stuttering Disorder / ChildhoodOnset Fluency Disorder
Disturbances in normal fluency and time patterning of speech
Social Pragmatic Communication Disorder
Deficits in verbal and nonverbal communication for social purposes
Lacks restricted/repetitive behaviors of ASD
Specific Learning Disorder
Diagnosis Criteria
Skills substantially lower than expected for age and intelligence
Onset during schoolage years
Types of Impairments
Reading
Written Expression
Mathematics
Severity
Mild, Moderate, Severe
Other Neurodevelopmental Conditions
Stereotypic Movement Disorder
Repetitive, seemingly driven, nonfunctional motor behavior
Onset in early developmental period
Neurocognitive Disorders
Distinct from neurodevelopmental disorders
Impact on independence in daily activities
Onset can be at any age, unlike neurodevelopmental disorders
Trauma and StressorRelated Disorder
Overview of TraumaRelated Disorders
Definition
Resulting from exposure to a traumatic or stressful event
Adjustment Disorder
Diagnostic Criteria
Development of emotional or behavioral symptoms in response to an identifiable stressor occurring within three months of its onset
Symptoms must be clinically significant marked distress or significant impairment in functioning
Key Insight 📅
Does not meet criteria for another mental disorder and is not an exacerbation of a preexisting mental disorder
Prognosis Insights
Good longterm prognosis for adult onset adolescent onset may progress to major psychiatric disorders
Acute Stress Disorder ASD
Diagnostic Criteria
Exposure to trauma with at least nine symptoms from five categories intrusion, negative mood, dissociative symptoms, avoidance, arousal
Duration is between three days and one month
Key Insight 🔑
Dissociative symptoms are a required criterion for ASD but a specifier for PTSD
PostTraumatic Stress Disorder PTSD
Diagnostic Criteria
Exposure to actual or threatened death, serious injury, or sexual violence, followed by symptoms from at least four clusters intrusion, avoidance, negative alterations in cognitions and mood, alterations in arousal and reactivity
Symptoms must persist for longer than one month
Specifiers 🧩
"With dissociative symptoms" depersonalization, derealization
"With delayed expression" full criteria not met until at least six months after trauma
Comorbidity Rates 📊
Very high, with 80% of individuals experiencing at least one other mental disorder commonly comorbid with MDD, SUDs, and anxiety disorders
Increased chronic risk of suicide and violence
ObsessiveCompulsive and Related Disorders
Overview of ObsessiveCompulsive Disorders
Characterization
Defined by the presence of obsessions recurrent, intrusive thoughts and/or compulsions repetitive behaviors aimed at reducing distress
Common Symptoms 🌀
Obsessions Contamination, pathological doubt, somatic concerns, symmetry, aggressive thoughts, sexual thoughts
Compulsions Checking, washing, counting, confessing, symmetry, hoarding
Subtypes
Earlyonset more severe, ticlike vs lateronset
Comorbidity Statistics 📈
High rates of comorbidity with anxiety disorders, major depressive disorder MDD, substance use disorders SUDs, Tourette's disorder, body dysmorphic disorder, and anorexia nervosa
In patients with Tourette's, OCD is common 35-50% conversely, Tourette's is less common in OCD 57%
Body Dysmorphic Disorder BDD
Diagnostic Criteria
Preoccupation with one or more perceived defects in physical appearance not observable or appearing slight to others
Involves repetitive behaviors or mental acts in response to appearance concerns
Hoarding Disorder
Diagnostic Criteria
Persistent difficulty discarding possessions due to perceived need to save them, leading to clutter that compromises intended use of living areas
Trichotillomania HairPulling Disorder
Diagnostic Criteria
Recurrent pulling out of one’s hair, resulting in hair loss repeated attempts to decrease or stop hair pulling
Excoriation SkinPicking Disorder
Diagnostic Criteria
Recurrent skin picking resulting in skin lesions repeated attempts to decrease or stop skin picking
Substance/MedicationInduced ObsessiveCompulsive and Related Disorder
Overview
Disorders arising from substance use or withdrawal that mimic OCD symptoms
Culture-Bound Syndromes
Patterns of symptoms or abnormal behavior recognized as illnesses in specific cultures (in ICD-10, coded under existing disorders like dissociative or somatoform).
A. Amok
Sudden onset of uncharacteristic psychomotor excitement with marked violence (homicidal/suicidal) and paranoid symptoms, followed by amnesia.
Described in Africa, Asia, New Guinea as a response to humiliation.
B. Ataque de Nervios
Hispanic American groups.
Common in Latin American cultures
Grief reaction with fluctuating conscious level (amnesia), crying, shouting, trembling, difficulty moving limbs.
Acute emotional disturbance
Hyperventilation may precipitate symptoms.
C. Latah
Asia and North Africa.
Found in Malaysia and Indonesia
Response to intense stress characterized by altered consciousness, hypersuggestibility, and mimicry (echolalia, echopraxia).
Characterized by sudden shouting or mimicry
D. Koro
Mainly Asia.
Seen in Southeast Asia
Intense anxiety centered on the belief that the genitalia are retracting and their disappearance will cause death.
Not delusional (associated with local tradition that ghosts have no genitals).
Fear of genital retraction
E. Brain Fag Syndrome
Mainly African students.
Concentration difficulties, vague somatic complaints, and depressed mood.
F. Piblokto (Arctic Hysteria)
Female Eskimos of northern Greenland.
Anxiety, depression, confusion, depersonalization, derealization, ending in stuporous sleep and amnesia.
G. Dhat Syndrome
South Asia.
Psychosexual disorder with anxiety about loss of semen.
H. Couvade Syndrome
Sympathetic pregnancy affecting husbands (rarely other family members) during their wives' pregnancies (most frequent between 3-9 months).
I. Windigo
Native American Indians.
Delusional fear of being turned into a cannibal through possession by a supernatural monster.
Feeding and Eating Disorders
Anorexia Nervosa
Bulimia Nervosa
Pica Persistent eating of nonnutritive, nonfood substances
Rumination Disorder Repeated regurgitation of food
Overview of Feeding and Eating Disorders
Definition
Involves persistent disturbance of eating or eatingrelated behavior leading to altered consumption or absorption of food, significantly impairing physical health or psychosocial functioning
Comorbidity Rates 📊
High rates of mood disorders 5070%), anxiety disorders 1365%), substance use disorders 25%), and personality disorders 2080%
Personality Disorders
Core Definition and General Criteria
Definition of Personality Disorder
Enduring pattern of inner experience and behaviour
Deviates from cultural expectations
Pervasive and inflexible across situations
Onset in adolescence or early adulthood
Stable over time
Leads to significant distress or impairment
Exclusion Criteria
Not better explained by another mental disorder
Not due to a medical condition
Not due to substance effects
DSM5TR Classification
Overview of DSM5TR
Retains 10 specific personality disorders from DSMIV
Grouped into three clusters
Cluster A Odd or Eccentric
Paranoid Personality Disorder
Distrust and suspiciousness
Interpretation of others' motives as malevolent
Schizoid Personality Disorder
Detachment from social relationships
Restricted emotional expression
Schizotypal Personality Disorder
Acute discomfort in close relationships
Cognitive or perceptual distortions
Eccentricities of behaviour
Cluster B Dramatic, Emotional, or Erratic
Antisocial Personality Disorder
Disregard for the rights of others
Criminality and impulsivity
Failure to learn from experience
Borderline Personality Disorder
Instability in relationships and selfimage
Marked impulsivity
Histrionic Personality Disorder
Excessive emotionality
Attention seeking behaviour
Narcissistic Personality Disorder
Grandiosity and need for admiration
Lack of empathy
Cluster C Anxious or Fearful
Avoidant Personality Disorder
Social inhibition and feelings of inadequacy
Hypersensitivity to negative evaluation
Dependent Personality Disorder
Submissive and clinging behaviour
Excessive need for care
ObsessiveCompulsive Personality Disorder
Preoccupation with orderliness and perfectionism
Control issues
Alternative DSM5 Model for Personality Disorders
Overview of Alternative Model
Hybrid dimensionalcategorical approach
Criterion A Impairments in Personality Functioning
Evaluated on a continuum mild to extreme
Selffunctioning identity and selfdirection
Interpersonal functioning empathy and intimacy
Moderate impairment required for diagnosis
Criterion B Pathological Personality Traits
Organized into five domains
Negative Affectivity
Detachment
Antagonism
Disinhibition
Psychoticism
Personality Disorder Trait Specified PDTS
For cases not meeting criteria for specific disorders
Significant impairment and pathological traits present
Sleep wake disorder
Overview of SleepWake Disorders
Definition and Impact
Persistent disturbances in sleepwake patterns causing distress or functional impairment
Affects quality of life and daily functioning
Insomnia Disorder 🌙
Criteria for Diagnosis
Predominant dissatisfaction with sleep quantity or quality
Difficulty initiating or maintaining sleep, or earlymorning awakening
Occurs at least 3 nights per week for a minimum of 3 months
Cooccurrence with Other Conditions
Often coexists with medical conditions, substance use disorders, or psychiatric disorders
Treatment should address both insomnia and cooccurring conditions for effective resolution
Hypersomnolence Disorder 😴
Criteria for Diagnosis
Excessive daytime sleepiness despite a main sleep period of at least 7 hours
Prolonged nighttime sleep or difficulty being fully awake after abrupt awakening
Occurs at least 3 times per week for a minimum of 3 months
Narcolepsy
Criteria for Diagnosis
Recurrent periods of an irresistible need to sleep, lapsing into sleep, or napping during the day
Occurs at least 3 times per week for a minimum of 3 months
Presence of cataplexy or specific hypocretin deficiency findings
Pathophysiology
Associated with a deficiency in hypocretin orexin, a neuropeptide that regulates wakefulness
BreathingRelated Sleep Disorders
Types of Disorders
Includes Obstructive Sleep Apnea Hypopnea, Central Sleep Apnea, and SleepRelated Hypoventilation
Diagnosis
Diagnosed based on polysomnographic criteria, assessing airflow and respiratory patterns during sleep
Circadian Rhythm SleepWake Disorders
Definition
Persistent or recurrent sleep disruption due to misalignment between the required sleepwake schedule and the individual's circadian rhythm
Examples
Shift work disorder, jet lag, and delayed sleep phase disorder
Parasomnias 😳
Characteristics
Abnormal behaviors, emotions, perceptions, or dreams occurring during sleep
Types of Parasomnias
NonREM Sleep Arousal Disorder Includes sleepwalking and sleep terrors
REM Sleep Behavior Disorder Involves repeated episodes of arousal during sleep associated with vocalization and complex motor behaviors
Often linked to synucleinopathies such as Parkinson's disease
Substance/MedicationInduced Sleep Disorder
Definition
Sleep disturbances caused by the effects of substances or medications
Examples
Alcohol, stimulants, and certain medications that interfere with normal sleep patterns
Disruptive, ImpulseControl, and Conduct Disorders
Psychopathology classification is a critical aspect of understanding mental health disorders, as it helps in diagnosing and treating individuals effectively The primary systems include the DSM5 Diagnostic and Statistical Manual of Mental Disorders and the ICD11 International Classification of Diseases Each framework categorizes disorders based on specific criteria, allowing professionals to communicate about mental illnesses more effectively This classification also aids in recognizing patterns in symptoms, guiding treatment plans, and facilitating research on the underlying causes of disorders However, it's essential to consider cultural and contextual factors when classifying psychopathology to ensure a comprehensive understanding of mental health
Overview of Disorders
Definition and Impact
Disorders characterized by problems in selfcontrol of emotions and behaviors
Can lead to significant social and personal issues
Oppositional Defiant Disorder ODD 😠
Criteria for Diagnosis
Pattern of angry/irritable mood, argumentative/defiant behavior, or vindictiveness lasting at least 6 months
Requires at least 4 symptoms eg, losing temper, easily annoyed, defying requests
Course and Prognosis
Approximately 25% will not have further diagnosis
30--40% of boys with severe ODD may progress to Conduct Disorder
Conduct Disorder CD
Criteria for Diagnosis
Repetitive and persistent pattern of behavior violating the basic rights of others or societal norms
Examples include aggression towards people or animals, destruction of property, deceitfulness, and serious rule violations
Important Note
Antisocial Personality Disorder ASPD requires a childhood diagnosis of conduct disorder for its diagnosis
Intermittent Explosive Disorder IED 💥
Criteria for Diagnosis
Recurrent behavioral outbursts representing a failure to control aggressive impulses
Outbursts are grossly out of proportion to the provocation and are not premeditated
Causes significant distress or impairment in functioning
Comorbidities
High rates of depression, anxiety, substance use disorders, ADHD, ODD, CD, ASPD, and borderline personality disorder
Kleptomania
Criteria for Diagnosis
Recurrent failure to resist impulses to steal objects not needed for personal use or monetary value
Increasing tension before the act and pleasure or relief during or after the act
Not committed out of anger or vengeance, and not explained by other disorders
Dissociative Disorrder
Dissociative Identity Disorder DID
Criteria and Features
Disruption of identity with ≥2 distinct personality states
Gaps in recall inconsistent with ordinary forgetting
DID takes precedence over other dissociative disorders if criteria are met
Dissociative Amnesia
Inability to recall important autobiographical information
Types localized, selective, generalized, and continuous amnesia
Differentiation from Neurocognitive Disorder NCD based on memory orientation
Depersonalization/Derealization Disorder
Persistent experiences of depersonalization or derealization
Reality testing remains intact can be distressing and trigger hypochondriacal concerns
Dissociative Disorders
Definition and Characteristics
Disruption in normal integration of consciousness, memory, identity, emotion, and behavior
Core etiology often linked to trauma eg, abuse, neglect
Symptoms typically begin in childhood, with a chronic course and high suicide attempt rates 70%
Assessment and Treatment
Rule out medical conditions and substance use
Treatment includes stabilization, psychotherapy, and grounding exercises
Avoid benzodiazepines, which may increase dissociation
Sexual disorders
Sexual Dysfunctions
Definition and Characteristics
Clinically significant disturbance in sexual response or pleasure
Heterogeneous group of disorders affecting sexual functioning
Examples include erectile dysfunction, premature ejaculation, and sexual aversion
Contributing Factors
Relationship problems, substances, and medical conditions
Psychological factors such as anxiety or depression can exacerbate dysfunction
Certain medications and chronic illnesses may also play a role
Paraphilic Disorders
Definition and Features
Recurrent, intense sexually arousing fantasies or behaviors
Involves nonhuman objects, nonconsenting individuals, or suffering/humiliation
Almost always affect males, with a maletofemale ratio of 201 for masochism
Diagnostic Criteria
Duration of ≥6 months causing distress or impairment
Fantasies or urges are sufficient for diagnosis even without acted behaviors
Often comorbid with other paraphilic disorders
Paraphilic Disorders
Overview of Paraphilic Disorders
Definition of Paraphilic Disorders
Paraphilic disorders involve intense sexual urges, fantasies, or behaviors that deviate from societal norms
These disorders often lead to distress or impairment in social, occupational, or other important areas of functioning
Diagnostic criteria are outlined in the DSM5, emphasizing the need for the behavior to cause significant distress or impairment
Prevalence and Impact
Paraphilic disorders are relatively rare but can have significant implications for individuals and society
Estimates suggest that around 510% of the population may experience some form of paraphilia
The impact on relationships, mental health, and legal issues can be profound, especially in cases involving nonconsensual acts
Types of Paraphilic Disorders
Voyeuristic Disorder 👀
Definition and Characteristics
Voyeuristic disorder involves observing unsuspecting individuals engaged in intimate behaviors
This can include watching others undress, engage in sexual activity, or use the bathroom
The individual experiences sexual arousal from these observations, often leading to distress or impairment
Legal and Ethical Considerations
Voyeurism can lead to legal consequences, including charges of invasion of privacy
Many jurisdictions classify voyeuristic behavior as a criminal offense, especially when it involves minors
Ethical concerns arise regarding consent and the rights of the observed individuals
Exhibitionistic Disorder 🎭
Definition and Characteristics
Exhibitionistic disorder involves exposing one's genitals to unsuspecting individuals for sexual gratification
This behavior may occur in public places or through digital means, such as sending unsolicited explicit images
The thrill of being seen or the shock value often contributes to the arousal experienced by the individual
Psychological Factors
Individuals may engage in this behavior due to underlying issues such as low selfesteem or a desire for control
Exhibitionism may serve as a coping mechanism for feelings of inadequacy or social anxiety
Treatment often focuses on addressing these underlying psychological factors
Frotteuristic Disorder 🚆
Definition and Characteristics
Frotteuristic disorder involves rubbing against a nonconsenting person for sexual pleasure
This often occurs in crowded places, such as public transport, where the individual can blend in
The act of touching or grinding against someone else provides a sense of thrill and excitement
Social Implications
Frotteurism can lead to significant distress for victims, who may feel violated or unsafe
Legal consequences can include charges of sexual assault or harassment
Awareness campaigns are essential to educate the public about consent and personal boundaries
Sexual Masochism Disorder 🔗
Definition and Characteristics
Sexual masochism disorder involves deriving sexual pleasure from being humiliated, beaten, or otherwise made to suffer
This can include a wide range of activities, from light bondage to more extreme forms of pain
The individual may seek out partners who are willing to engage in these activities consensually
Consent and Safety
Consent is a critical component of sexual masochism, distinguishing between healthy practices and abusive behavior
Safe words and clear communication are essential to ensure the wellbeing of all parties involved
Education on BDSM practices emphasizes the importance of mutual consent and safety measures
Sexual Sadism Disorder 🔥
Definition and Characteristics
Sexual sadism disorder involves deriving sexual pleasure from inflicting pain or humiliation on others
This can manifest in various ways, including physical violence or psychological manipulation
The behavior becomes a disorder when it causes distress or impairment to the individual or their partner
Ethical Considerations
The line between consensual sadism and abuse can be blurred, raising ethical concerns
It is crucial to differentiate between consensual BDSM practices and nonconsensual acts of violence
Discussions around consent and power dynamics are essential in understanding sexual sadism
Fetishistic Disorder 👗
Definition and Characteristics
Fetishistic disorder involves sexual arousal from nonliving objects or specific body parts
Common fetishes include clothing items eg, lingerie, leather or body parts eg, feet
The fetish becomes a disorder when it significantly impairs functioning or causes distress
Cultural Perspectives
Fetishes can vary widely across cultures and may be influenced by societal norms and values
Understanding the cultural context of fetishes is essential for a comprehensive view of human sexuality
Some fetishes are more accepted in certain cultures, while others may be stigmatized
Transvestic Disorder 🌈
Definition and Characteristics
Transvestic disorder involves sexual arousal from crossdressing, typically associated with heterosexual males
The behavior may include wearing clothing typically associated with the opposite gender
This disorder is characterized by distress or impairment related to the crossdressing behavior
Gender Identity and Expression
Transvestism is distinct from transgender identity many individuals may crossdress without identifying as transgender
Understanding the nuances of gender identity is crucial in discussions about transvestic disorder
Support and acceptance are essential for individuals exploring their gender expression
Pedophilic Disorder 🚸
Definition and Characteristics
Pedophilic disorder involves sexual attraction to prepubescent children, typically 13 years old or younger
This disorder is considered one of the most serious due to the potential for exploitation and harm to minors
The individual may act on these urges or experience significant distress due to them
Legal and Social Implications
Pedophilia is illegal and heavily stigmatized, leading to severe legal consequences for offenders
Societal attitudes towards pedophilia are overwhelmingly negative, reflecting a strong protective instinct for children
Treatment options focus on managing urges and preventing harmful behaviors, often involving therapy and support groups
Gender Dysphoria
Definition and Key Concepts
Marked incongruence between experienced gender and assigned gender
Chief diagnostic concept gender incongruence
May lead to significant distress or impairment in social, occupational, or other areas of functioning
Differential Diagnosis
Distinguishing from other disorders
Simple gender nonconformity in children
Body Dysmorphic Disorder and Schizophrenia delusional
Transvestic disorder focuses on sexual arousal rather than gender incongruence
Somatic Symptom related disorder
Somatic Symptom and Related Disorders
Definition and Characteristics
Somatic symptoms causing significant distress or functional impairment
DSM5 no longer emphasizes "medically unexplained symptoms"
Patients can have concurrent medical diagnoses and somatic symptom disorders
Comorbidities and Treatment
High rates of mood disorders 60% and anxiety disorders 50%
Treatment focuses on "care not cure," emphasizing longterm relationships with clinicians
Useful therapies include psychotherapy CBT and pharmacotherapy antidepressants
Psychological Factors Affecting Other Medical Conditions
Psychological factors adversely affecting a medical condition
Influences course, treatment, and pathophysiology of the medical condition
Factitious Disorder
Falsification of symptoms or induction of injury/disease
Distinction from malingering no external incentive for deception
Management focuses on safety and care rather than confrontation
Conversion Disorder
Symptoms of altered voluntary motor or sensory function
Acute onset often linked to stressors short duration of episodes
Treatment involves suggestion therapy and ongoing CBT
Illness Anxiety Disorder IAD
Preoccupation with serious illness despite mild or absent somatic symptoms
Excessive healthrelated behaviors or maladaptive avoidance
Duration of ≥6 months
Somatic Symptom Disorder SSD
Criteria and Specifiers
≥1 distressing somatic symptom with excessive thoughts or behaviors related to health concerns
Specifier "With predominant pain" when symptoms primarily involve pain
Due to another medical condition
Substance use disorder
Dx Criterion
Two or more during 12 months
1. Tolerance
2. Withdrawal
3. Unable to Control use
4. Waste a lot of time to obtain/ use/ recover
5. Craving
6. Social occupational decline
Mood disorders
Depressive Disorders
Major Depressive Disorder MDD 😞
Criteria ≥5 symptoms present nearly every day for 2week period, with at least depressed mood or anhedonia
Specifiers
With Melancholic Features Loss of pleasure in all/almost all activities, lack of reactivity to pleasurable stimuli
With Atypical Features Mood reactivity is key Also, ≥2 of hypersomnia, increased appetite/weight gain, leaden paralysis, sensitivity to interpersonal rejection MCQ Point Classically responds to MAOIs
With Psychotic Features Delusions or hallucinations are present Can be moodcongruent themes of guilt, deserved punishment or moodincongruent persecutory, grandiose Treatment Antidepressant + Antipsychotic or ECT
With Catatonia ≥3 catatonic symptoms eg, stupor, catalepsy, mutism, waxy flexibility, echolalia, echopraxia
With Peripartum Onset Onset during pregnancy or within 4 weeks postpartum
With Anxious Distress
With Mixed Features
Comorbidities Very high lifetime comorbidity 72% with any other mental disorder Most frequent in pediatric depression Anxiety GAD, Panic, Disruptive Behavior Disorders ODD, CD, ADHD, Substance Use Disorders
Age of onset
Average Age of Onset: 29 years.
Onset in Younger Populations:
◦ 2% prevalence in children.
◦ 4-8% prevalence in adolescents.
◦ Approximately 20% lifetime prevalence by age 18.
Major Depressive Disorder (MDD) Onset Age detail
Normal Age of Onset
Overall Range
MDD can occur at any age, from childhood to old age
Peak Incidence
Most common onset in the 20s
Median age of onset 25 years or late 20s
Peak risk midtolate adolescence through early 40s
Recurrent MDE average onset 30 to 35 years
Bimodal Pattern
Two peaks early adulthood and later life/middle age after 40 years
Onset in Specific Age Groups
Childhood/Prepubertal Onset
Prevalence & Presentation
MDD rarely diagnosed in early childhood mild symptoms can appear
Symptoms
Irritable mood may replace depressed mood symptoms vary with cognitive development
Prevalence in Youth
05% in preschoolers, 12% in schoolaged children, 4 to 11% in adolescents
Adolescent Onset
Increased Likelihood
MDD onset likelihood increases with puberty
Gender Differences
Higher femaletomale ratio begins in early adolescence
Prognosis
Strong risk of recurrence in adult life
Late Life/Older Adults Onset
Prevalence
First onset in late life is common higher in nursing home residents
Association with Medical Causes
Onset between 45 and 65 years often linked to medical causes newonset after 60 prompts medical evaluation
Prognostic Factors
Less family history of mood disorders higher dementia prevalence milder and chronic less common first episodes after 60
Late-Onset Depression: This is defined as the initial onset at 65 years or older.
Key Features & Course Related to Onset
Kindling Phenomenon
Early episodes triggered by life stressors later episodes may occur without clear triggers
Impact of Early Onset
Negative predictor
More severe symptoms
Increased comorbid physical and mental illnesses
Higher risk of recurrent episodes
Increased suicide attempt risk
Poorer social outcomes eg, loneliness, never marrying
More severe developmental course
Persistent Depressive Disorder Dysthymia
Disruptive Mood Dysregulation Disorder DMDD 🎭
Criteria Severe recurrent temper tantrums verbal/behavioral, disproportionate ≥3x/week Mood between tantrums persistently irritable/angry Present for ≥12 months in ≥2 settings MCQ Point Age of onset before 10 years Do not diagnose before age 6 or after age 18 Cannot be comorbid with ODD, Bipolar, or IED
Depressive Disorders Assessment and Treatment
Assessment Comprehensive psychiatric, physical/neurological exams Screen for substance abuse, assess suicide/homicide risk Obtain detailed family history Information from multiple sources parents, teachers
Psychotherapies Cognitive Behavioral Therapy CBT, Interpersonal Psychotherapy IPT, ProblemSolving Therapy PST, Psychodynamic Psychotherapy
Medication Risk Black Box Warning for antidepressants increasing the risk of suicidal thinking and behavior suicidality in children, adolescents, and young adults in shortterm studies
Bipolar and Related Disorders
Overview of Bipolar Disorders
Definition and Characteristics
Distinct periods of abnormally elevated, expansive, or irritable mood and increased activity or energy 🌈
Bipolar I Disorder
Diagnostic Criteria
At least one manic episode required for diagnosis
Marked impairment in social or occupational functioning differentiates it from hypomania
Manic Episode Features
Distinct period of elevated mood for ≥1 week or any duration requiring hospitalization
Symptoms include grandiosity, decreased sleep, talkativeness, distractibility, and increased activity
Epidemiology and Prognosis
Average age of onset is 19 years significant suicide risk up to 50% attempt, 15% complete
Psychotic symptoms are common in 50% of cases
Bipolar II Disorder
Diagnostic Criteria
At least one hypomanic episode and one major depressive episode required
No manic episodes present
Features
Depression is more prominent than hypomania comparable suicide rates to Bipolar I
Rapid cycling is common, indicating frequent mood changes
Cyclothymic Disorder
Diagnostic Criteria
Numerous periods with hypomanic and depressive symptoms for ≥2 years ≥1 year for children/adolescents
Symptoms present at least half the time no major depressive, manic, or hypomanic episodes ever met 🌀
must never have been without symptoms for more than 2 months at a time
Age of onset: 15-25
Prevalence: 1% – M:F 1:1 in general population
Secondary Bipolar Disorders
Substance/MedicationInduced Bipolar Disorder
Mood disturbance directly from substance intoxication, withdrawal, or medication use
Medications like corticosteroids, antidepressants, and stimulants can induce mania
Dopamine agonists
L-DOPA
Sympathomimetics
Amphetamine
Cocaine
Pseudoephedrine
PCP
Antibiotics
◦ Ciprofloxacin
Clarithromycin
Anabolic and corticosteroids
Bipolar Disorder Due to Another Medical Condition
Direct pathophysiological consequence of a medical condition eg, CVA, seizure disorders
Differentiation from primary mania based on age of onset and related medical causes
Other Specified Bipolar and Related Disorder
Criteria for Diagnosis
Symptoms cause distress but do not meet full criteria for specific bipolar disorders
Examples include shortduration hypomanic episodes with major depressive episodes
Bipolar and Related Disorders Treatment Principles Pediatric Focus
Acute Mania/Mixed Episodes
Mood stabilizers Lithium, Valproic Acid or atypical antipsychotics Olanzapine if no psychosis
If psychosis present, combine mood stabilizer with atypical antipsychotic
Lithium Treatment
FDAapproved for ages 1217 requires regular renal and thyroid function tests
Atypical Antipsychotics
Risperidone approved for ages 1017 monitoring for weight gain, sedation, and metabolic side effects
Bipolar Depression Management
OlanzapineFluoxetine combination Symbyax, Quetiapine, Lurasidone are effective treatments
Caution with antidepressants due to risk of inducing mania
Rapid Cycling Management
Stop antidepressants optimize mood stabilization with Valproate over Lithium 🔄
Star D response Rate
what is response?
more than 50 % score improvement in HAM-D17
what is remission?
what is partial remission
50 % decrease in HAMD 17 score but total score is above 7.
20%-40% pts after the initial trial
– 76% of partial remitters relapsed by month 15
Secondary Depressive Disorders
Due to Another Medical Condition Examples include AIDS, Lupus, Poststroke, Thyroid disease, Parkinson's, Huntington's, Alzheimer's, TBI, Obstructive Sleep Apnea
that is a direct pathophysiological consequence of another medical condition
vs Distinguish from
Adjustment Disorder: It's not just a psychological reaction to coping with a medical illness
Presence of atypical features of depression (e.g., unusual age of onset, absence of family history) can suggest a medical cause
Substance/MedicationInduced Due to prominent and persistent depressed mood or diminished interest/pleasure directly from substance/medication
Agent Capability
Alcohol: Most common legal depressant;
intoxication and withdrawal
Benzodiazepines
cause depressant effects; withdrawal can also induce depressive symptoms
Barbiturates: Known depressants
Hypnotics: Can lead to low mood; withdrawal can cause depression
Opioids/Opiates
Can cause depressive syndromes; withdrawal leads to dysphoric mood
Gammahydroxybutyrate (GHB)
Stimulants (mainly during withdrawal)
Amphetamines.
Nicotine (withdrawal)
Antihypertensive Agents
affecting catecholamine levels
Reserpine:
A classic MCQ culprit. It depletes monoamines (dopamine, norepinephrine, serotonin) and is a recognized cause of depression and suicide
Methyldopa
Clonidine
Hormonal agent
Corticosteroids / Steroids: Very commonly implicated in inducing depression (as well as euphoria, mania, or psychosis)
Oral Contraceptives
Thyroid Hormone (Dysregulation)
(e.g., hypothyroidism) can cause depressive symptoms
Antimicrobial
Isoniazid
Cephalosporins
Quinolones (e.g., Ciprofloxacin)
Temporal Relationship: Symptoms develop during or soon after substance intoxication, withdrawal, or medication exposure/change/withdrawal
Persistence:
If symptoms persist for a substantial period (e.g., about 1 month) after cessation of acute withdrawal or severe intoxication, it strongly suggests an independent depressive disorder rather than purely substance-induced. This distinction is frequently tested.
Meds/ Organic/ Substance associated Depressive Disorder
Diagnosis Depression Due to Another Medical Condition
Core Criteria
Prominent and persistent depressed mood
Diminished interest or pleasure in activities
Direct pathophysiological consequence of another medical condition
Not better explained by another mental disorder
Does not occur exclusively in delirium
Infectious Diseases
Neurosyphilis
AIDS
Secondary Depression Medical Etiologies
Neoplasms
Brain tumors
Pancreatic cancer
Paraneoplastic syndromes
Immune Disorders
AIDS
Systemic lupus erythematosus
Cardiac Conditions
Poststroke
Postmyocardial infarction MI
Coronary heart disease
Endocrine Disorders
Thyroid disease
Cushing’s syndrome
Neurologic Disorders
Multiple sclerosis
Epilepsy
Parkinson’s disease
Huntington’s disease
Alzheimer’s disease
Traumatic brain injury
Stroke
Other Conditions
Obstructive sleep apnea
Diagnosis Substance/MedicationInduced Depressive Disorder
Core Criteria
Prominent and persistent depressed mood
Symptoms develop during or within a month of substance use
Substance capable of producing depressive symptoms
Types of Substances
Illicit drugs
Prescription medications
Drugs of Abuse Inducing Depression
Alcohol
Phencyclidine
Hallucinogens
Inhalants
Opioids
Sedative, hypnotic, anxiolytic
Amphetamines or stimulants
Cocaine
Other or unknown substances
Medications Associated with Depression
Acyclovir
Anabolic steroids
ACE inhibitors
Anticonvulsants
Baclofen
Barbiturates
Benzodiazepines
βBlockers
Bromocriptine
Calcium channel blockers
Ciprofloxacin
Clonidine
Corticosteroids
Digitalis
Disulfiram
Estrogen
Guanethidine
H2 receptor blockers
Interferon α
Interleukin2
Isotretinoin
Levodopa
Methyldopa
Metoclopramide
Metrizamide
Metronidazole
NSAIDs indomethacin
Opioids
Pergolide
Reserpine
Sulfonamides
Thiazide diuretics
Topiramate
Vinblastine
Vincristine
Psychotic disorders
Schizophrenia and Psychotic Disorders: Core Review for MCQ Exam Preparation
I Defining Psychosis & Key Symptom Domains
Psychosis Definition
A mental state with grossly distorted reality, leading to delusions, hallucinations, and thought disorder
Five Key Symptom Domains DSM5TR
1 Delusions
2 Hallucinations
3 Disorganized Thinking Speech
4 Grossly Disorganized or Abnormal Motor Behaviour including Catatonia
5 Negative Symptoms
II Symptoms and Presentation
Delusions
Fixed, false beliefs resistant to change despite evidence
Common Types
Persecutory
Referential
Grandiose
Erotomanic
Nihilistic
Infidelity Jealous
Somatic
Hallucinations
Perceptual experiences without external stimuli
Types
Auditory most common
Visual
Other Modalities Tactile, Olfactory, Gustatory
Negative Symptoms
Deficits in normal functioning, often treatmentresistant
Key "A"s Four As
Apathy
Alogia
Avolition
Affective Blunting/Flattening
Catatonia
Neuropsychiatric syndrome with psychomotor disturbances
Manifestations
Stupor
Catalepsy
Waxy flexibility
Mutism
Negativism
Posturing
Mannerism
Stereotypy
Agitation
Echolalia
Echopraxia
Grimacing
III Subtypes/Related Conditions
Schizophrenia
Chronic disorder with thought, emotion, and behavior abnormalities
Diagnostic Criteria DSM5
2+ symptoms for 1+ month
Continuous signs for 6+ months
Chronic Schizophrenia
Persistent disability for 2+ years, with negative symptoms predominating
Schizoaffective Disorder
Concurrent symptoms of schizophrenia and a major mood episode
Delusional Disorder
Presence of 1+ delusions for 1+ month without core schizophrenic symptoms
Prognostic Factors in Schizophrenia
I Prognosis in Schizophrenia Subtypes
A Paranoid Subtype Best Prognosis
1 Outcome
Best outcome and better prognosis among all subtypes
Better outcome than simple type
2 Onset
Later age of onset
Develops rapidly or acutely in individuals with good premorbid functioning
3 Symptoms
Prominent delusions persecutory or grandiose and auditory hallucinations
Negative symptoms and thought disorganization are not prominent
Relatively preserved affect and cognitive functions
4 Course
Intermittent course during the first 5 years
Less personality deterioration compared to other types
B Other Subtypes
1 Disorganized Hebephrenic Subtype
Worst prognosis
Earlier onset 1525 years and insidious course
Early negative symptoms
2 Undifferentiated Subtype
Intermediate prognosis
3 Catatonic Subtype
Generally considered to have a good outcome
II General Prognostic Factors in Schizophrenia
A Good Prognostic Factors
1 Demographic & Social
Later age of onset
Female gender
Being married
Good social support/network and social contacts outside the home
Higher IQ / high premorbid intelligence
Living in developing countries
2 Illness Characteristics
Acute/abrupt onset of prominent psychotic symptoms within 4 weeks
Obvious precipitating factors/stressors eg, life stress
Good premorbid social and occupational functioning/adjustment
Presence of positive symptoms
Presence of affective symptoms depression or elation
Family history of mood disorders not schizophrenia
Short duration of illness prior to treatment / short duration of untreated psychosis DUP
Confusion or perplexity at height of psychotic episode
Absence of blunted or flat affect
3 Treatment Response
Good initial response to treatment best predictor
Good response to medication
B Poor Prognostic Factors
1 Demographic & Social
Younger age of onset
Male gender
Being single, divorced, or widowed
Poor social network/social withdrawal/isolation
Minority status
2 Illness Characteristics
Insidious/gradual onset
No precipitating factors
Poor premorbid adjustment/functioning
Prominent negative/deficit symptoms
Family history of schizophrenia weak, controversial
Longer duration of initial episode/untreated psychosis DUP
Many relapses/chronic course/no remissions in 3 years
Low IQ
3 Comorbidities
Substance abuse eg, cannabis use
Other comorbid disorders eg, obsessivecompulsive symptoms, aggressive behavior, depression
History of violence
4 Other Factors
Neurological signs and symptoms eg, soft neurological signs, cognitive symptoms, ventricular enlargement
Poor compliance to medication
Poor social network, high Expressed Emotion EE families
History of perinatal trauma
Poor insight
III Factors NOT Associated with Prognostic Significance
A First Rank Symptoms FRS
Do not carry prognostic significance in schizophrenia
B Positive response to placebo
C Being female
Inconsistent association with prognosis in some longerterm predictions
Contradicts other sources stating female gender is a good prognostic factor
Suggests unresolved issues regarding family history of mood disorders and age of onset
IV Prognostic Factors for Paranoid Schizophrenia & Age of Diagnosis
Prognostic Factors
Best outcomes associated with
Later Age of Onset
Acute/Rapid Onset
Good Premorbid Functioning
Age of Diagnosis
Typical onset late teens to mid30s earlier onset indicates poorer prognosis
V Suicide Risk Factors in Schizophrenia
Lifetime Risk
56% complete suicide up to 20% attempt
Specific Risk Factors
Young Age
Male Gender
High Premorbid Functioning
Poor Compliance with Treatment
Comorbid Depression
Command Hallucinations
Recent Psychotic Episode
Unemployment
Greater Insight into Illness
Lack of Social Support
B. Specific Delusional Syndromes
Cotard's Syndrome
Patient's belief that they do not exist, that part of their body is not there (nihilistic delusion), or that they are dead.
Associated with severe depression and psychotic disorders.
Capgras Syndrome (Delusion of Doubles)
Belief that familiar persons have been replaced by identical imposters or strangers in disguise.
Fregoli Syndrome
Belief that a familiar person is able to change their appearance or is in disguise, often with persecutory themes.
De Clerambault's Syndrome (Erotomania)
Delusion that another person, usually of higher status, is in love with the patient.
Othello Syndrome (Morbid Jealousy)
Delusional jealousy.
Charles-Bonnet Syndrome (CBS)
Persistent or recurrent complex hallucinations (usually visual or auditory) occurring in clear consciousness, typically against a background of visual impairment (not mandatory).
Insight is usually preserved, and no other significant neuropsychiatric disturbance.
Associated with age-related macular degeneration.
EKBOMB
C. Catatonia
Syndrome of primarily psychomotor disturbances (stupor, catalepsy/waxy flexibility, mutism, negativism, posturing, mannerisms, stereotypies, psychomotor agitation, grimacing, echolalia, echopraxia, ambitendency).
Bell Mania: Disorganized hyperactivity (vs. waxy flexibility/rigidity in lethal catatonia).
Gjessing Syndrome: "Periodic catatonia" - disorganized state of withdrawal or agitation that fluctuates.
Diagnosis and Symptoms
Requires ≥3 catatonic symptoms can be added to any mental disorder diagnosis
Treatment
Firstline treatment is Lorazepam avoid antipsychotics until catatonia resolves
ECT may be used for refractory cases
Schizoaffective Disorder
Diagnostic Criteria
Major mood episode concurrent with schizophrenia criteria delusions or hallucinations present for 2+ weeks without mood episode
Prognosis
Better than schizophrenia but worse than mood disorders more psychotic symptoms predict poorer prognosis
Delusional Disorder
Diagnostic Criteria
Presence of one or more delusions for ≥1 month functioning not markedly impaired
presence of delusions without other prominent psychotic symptoms like hallucinations (if present, they are related to the delusion and not prominent), disorganized speech, or negative symptoms,
Patients generally maintain good functioning outside the direct impact of their delusion and their behavior is not overtly bizarre
Tends to be stable over time. Less than 25% progress to schizophrenia, and less than 10% develop a mood or bipolar disorder
Subtypes and Treatment
Subtypes include erotomanic, grandiose, and persecutory treatment includes antipsychotics
Patients often resistant to treatment but prognosis better than schizophrenia
Schizophrenia
Diagnostic Criteria
At least two characteristic symptoms for ≥1 month delusions, hallucinations, or disorganized speech
Continuous signs of disturbance for at least 6 months
Positive and Negative Symptoms
Positive Delusions, hallucinations, disorganized behavior
Negative Diminished emotional expression, social withdrawal, lack of spontaneity
Epidemiology and Prognosis
Lifetime prevalence ~1% peak onset in males 1525 years and females 2535 years
Severity inversely related to age of onset negative symptoms predict poorer outcomes
Overview of Psychotic Disorders
Definition and Characteristics
Involve a break from reality, often with delusions or hallucinations 🌌
Other Specified/Unspecified Psychotic Disorder
Other Specified
Psychotic symptoms causing distress without meeting specific disorder criteria
Unspecified
Distress from psychotic symptoms without clear criteria for diagnosis
Schizophreniform Disorder
Diagnostic Criteria
Symptoms same as schizophrenia for ≥1 month but less than 6 months
Prognostic Features
Good prognosis if symptoms appear within 4 weeks of behavior change and good premorbid functioning
Over 50% may progress to schizophrenia diagnosis
Brief Psychotic Disorder
Diagnostic Criteria
Positive symptoms for ≥1 day but less than 1 month with full return to premorbid functioning
Prognosis
4050% may progress to another psychotic illness, commonly schizophrenia
Psychotic Disorder Due to Another Medical Condition
Criteria
Prominent hallucinations or delusions as a direct consequence of a medical condition
Substance/MedicationInduced Psychotic Disorder
Criteria
Delusions or hallucinations during or soon after substance intoxication/withdrawal
Differentiation
Persistent symptoms suggest primary psychotic disorder if they last ~1 month postintoxication
Another medical illness
Restless Legs Syndrome (RLS) Diagnosis and Treatment
Diagnosis Criteria
Core Symptoms
Urge to move legs with uncomfortable sensations
Characteristic Features
Onset/Worsening at Rest
Begins or worsens during inactivity
Relief by Movement
Urge is partially or totally relieved by movement
Diurnal Pattern
Symptoms worse in evening/night than during the day
Frequency and Duration
Occurs at least 3 times per week for 3 months
Exclusionary Criteria
Not attributable to other conditions
Anemia
Peripheral neuropathy
Diabetes
Akathisia from dopamine antagonist medication
Distinction from akathisia inner feeling of restlessness
Treatment Approaches
Pharmacological Management
Firstline Agents FDA Approved Dopamine Agonists
Ropinirole Requip
Pramipexole Mirapex
Rotigotine Neupro transdermal system
Severe Cases Treatment
Carbidopa/levodopa as drug of choice
Secondline Agents
Benzodiazepines
Clonazepam
Opiates
Methadone
Codeine
Oxycodone
Other Medications
Bromocriptine
Clonidine
Carbamazepine
Baclofen
NonPharmacological / Lifestyle Modifications
Avoidance Strategies
Avoid alcohol
Avoid caffeine
Avoid nicotine
Considerations
Vitamin supplements
Physical therapy
Stretching
Exercise
SSD
PTSD
hypoparathyroidism
Etiology;
parathyroid gland injury or accidental removal during thyroid surgery (iatrogenic)
also be due to genetic and autoimmune diseases
Biochemical Features:
low or undetectable PTH levels
Leading to Low serum calcium levels
Elevated phosphate levels
Low levels of 1,25-dihydroxy vitamin D
Associated Physical Signs & Symptoms
Neuromuscular irritability
Paresthesia
Muscle cramps
Tetany
(e.g., carpopedal spasm, laryngospasm) Occurs especially if calcium level decreases suddenly
Clinical Signs
Chvostek's Sign
Contraction of facial muscles upon tapping the facial nerve
Trousseau's Sign
Carpal spasm induced by inflating a blood pressure cuff
Seizures
Other Neurological/Systemic:
Extrapyramidal symptoms
Increased intracranial pressure
Basal ganglia calcifications
Cardiac arrhythmias
prolonged QT interval
Skin changes
(dry, scaly, pigmented skin; brittle nails; coarse/thin hair; alopecia)
Psychiatric Manifestations
directly proportional to serum calcium levels, worsening as hypocalcemia becomes more severe
Mood Disorders:
Depression
Frequently reported and its incidence is increased
Emotional Lability
Common in patients with mild hypocalcemia
Mania: Can occur in severe cases
Anxiety Syndromes:
Common manifestation
Irritability Frequently noted
especially in mild hypocalcemia
Psychotic Features:
Can develop in severe hypocalcemia
Cognitive Disorders
Most frequently encountered syndrome
Cognitive impairment and dysfunction
Ranges from mild subjective slowing to severe delirium and encephalopathy
Brain fog
its severity is proportional to calcium concentration and duration of the disease
Management
Correction of the calcium level (along with vitamin D and magnesium) is the primary and first step
Parenteral calcium and magnesium replacement
Prognosis
Psychiatric symptoms usually improve rapidly or resolve with treatment of the underlying hypoparathyroidism and normalisation of calcium levels
If psychotic symptoms persist after addressing the hypoparathyroidism, consider Adjunctive Treatment: adding an antipsychotic like haloperidol
Biochemical manifestation of disease
Low vitamin D
high po4
low ca
Subtopic
Etiology bandage on the neck
And scrub
Clinical sign
C on cheek
T on Arm BP cuff
Crab is equal to cramp
Ants and stars paresthesia
Rope on the neck show laryngospasm)
Rope on the wrist show carpopedal spasm)
Treatment. Drip set. Calcium and magnesium correction IV
Pheochromocytoma Diagnosis
II Laboratory Confirmation
A Diagnostic Goal
1 Proof of excessive catecholamine release before anatomical localization
B Preferred Initial Test
1 Plasma Free Metanephrines
a More specific and convenient than urine testing
b Blood can be drawn at any time
c Positive Result Plasma levels >2 times upper limit of normal
C Alternative Test
1 Fractionated 24hour Urine Metanephrines
a Used for lower risk patients
b Positive Result Urine metanephrine levels ≥3 times upper reference limit
c Urinary Vanillylmandelic acid VMA as a metabolite for screening
D Crucial Considerations for Lab Testing
1 Drug Interference
a Falsepositive results from various medications
i Dopamine D2blocking antipsychotics
ii Tricyclic Antidepressants TCAs
iii SNRIs
iv MAOIs
v Cocaine, ketamine, sympathomimetics
vi Nonselective βblockers
vii Prazosin
viii Certain hormones and anesthetic agents
2 Preparation for Testing
a Interfering drugs must be discontinued at least 2 weeks prior
b 3day diet free of specific foods recommended
3 Physical Activity
a Intense physical activity can cause minor elevations
I Clinical Suspicion
A Classic Triad
1 Episodic headache
2 Sweating diaphoresis/hyperhidrosis
3 Tachycardia
B Hypertension
1 Labile hypertension
2 Severe, variable hypertension
3 Difficulttomanage hypertension
4 Norepinephrinesecreting tumors causing baseline hypertension
C Psychiatric Mimicry
1 Symptoms mimic panic attacks or generalized anxiety disorder GAD
2 Key Discriminator Panic attacks with headache, palpitations, blood pressure abnormalities, diaphoresis
D Other Red Flags
1 Nervousness, tremulousness
2 Hyperglycaemia
3 Abdominal or chest pain
4 Nausea, vomiting, weakness
5 Pallor rarely flushing
E Precipitating Factors/Triggers
1 Postural changes
2 Abdominal compression or tumor palpation
3 Emotional trauma
4 Induction of anesthesia
5 Unopposed beta blockade
6 Urination if bladder tumor
7 Certain medications or foods high in tyramine
F Family History
1 Onethird of cases part of hereditary syndromes eg, MEN2, vHL, NF1
III Anatomical Localization
A Purpose
1 Imaging studies performed to localize the tumor after biochemical confirmation
B Imaging Modalities
1 CT Scan
a Costeffective and widely available
b Better spatial resolution
2 MRI
a Preferred for children and pregnant individuals
b Absence of radiation exposure
C Specialized Imaging
1 123IMIBG scintigraphy or PET scanning for occult or metastatic tumors
Anxiety disorders
Hyperthyroidism
pheochromocytoma
asthma
hypertension
ulcers
arthritis
Corticosteroids
Obsessive-Compulsive and Related Disorder
Huntington's disease
cerebral infarction
Disorders leading to striatal damage
Personality Change:
neoplasms
head trauma
cerebrovascular disease
Huntington's
epilepsy
Catatonic Disorder
C. Catatonia
Syndrome of primarily psychomotor disturbances (stupor, catalepsy/waxy flexibility, mutism, negativism, posturing, mannerisms, stereotypies, psychomotor agitation, grimacing, echolalia, echopraxia, ambitendency).
Bell Mania: Disorganized hyperactivity (vs. waxy flexibility/rigidity in lethal catatonia).
Gjessing Syndrome: "Periodic catatonia" - disorganized state of withdrawal or agitation that fluctuates.
Depressive Disorder
CVA/stroke
Huntington's disease
Parkinson's disease
TBI
Cushing's syndrome
hypothyroidism
autoimmune disorders
B12 deficiency
MS
A. Psychiatric Syndromes Due to General Medical Conditions
Cushing's Syndrome: Can cause bipolar disorder, depression (in ~60% of patients), mania, or psychosis (resembling steroid psychosis).
Systemic Lupus Erythematosus (SLE) / Cerebral Lupus: Can present with psychiatric problems ("lupus psychosis"), anxiety, or mood disorders.
Acute Intermittent Porphyria (AIP): Autosomal dominant. Can cause intermittent attacks of abdominal pain, polyneuropathy, seizures, delirium, anxiety disorders ("Great Imitator").
Hyperthyroidism: Most common psychiatric manifestation is anxiety disorder. Can also cause psychosis.
Hypothyroidism: Most commonly reported psychiatric symptom is depression. Can also cause psychosis ("myxoedema madness").
HIV-associated Dementia (HAD) / AIDS Dementia Complex (ADC): Cognitive, affective, behavioral, motor dysfunction (impairments in attention, memory, motor speed). Common complication of late untreated HIV disease.
AI
SLE
Subtopic
OCD
Hoarding Disorder
Diagnostic Criteria
Persistent difficulty discarding possessions due to perceived need to save them, leading to clutter that compromises intended use of living areas
Body Dysmorphic Disorder BDD
Diagnostic Criteria
Preoccupation with one or more perceived defects in physical appearance not observable or appearing slight to others
Involves repetitive behaviors or mental acts in response to appearance concerns
Treatment Recommendations 💡
Cognitive Behavioral Therapy CBT and serotonergic antidepressants are recommended
Overview of ObsessiveCompulsive Disorders
Characterization
Defined by the presence of obsessions recurrent, intrusive thoughts and/or compulsions repetitive behaviors aimed at reducing distress
Common Symptoms 🌀
Obsessions Contamination, pathological doubt, somatic concerns, symmetry, aggressive thoughts, sexual thoughts
Compulsions Checking, washing, counting, confessing, symmetry, hoarding
Subtypes
Earlyonset more severe, ticlike vs lateronset
Comorbidity Statistics 📈
High rates of comorbidity with anxiety disorders, major depressive disorder MDD, substance use disorders SUDs, Tourette's disorder, body dysmorphic disorder, and anorexia nervosa
In patients with Tourette's, OCD is common 3550% conversely, Tourette's is less common in OCD 57%
Treatment Modalities
Medication
SSRIs are the firstline pharmacologic treatment for OCD
Psychotherapy
Cognitive Behavioral Therapy CBT with Exposure and Response Prevention ERP is highly effective
Treatment Duration Insight
For patients with a good medication response, fulldose medications should be continued for at least 12 years before considering discontinuation
Trichotillomania HairPulling Disorder
Diagnostic Criteria
Recurrent pulling out of one’s hair, resulting in hair loss repeated attempts to decrease or stop hair pulling
Treatment Focus
Habit reversal training is the most effective behavioral therapy
Excoriation SkinPicking Disorder
Diagnostic Criteria
Recurrent skin picking resulting in skin lesions repeated attempts to decrease or stop skin picking
Substance/MedicationInduced ObsessiveCompulsive and Related Disorder
Overview
Disorders arising from substance use or withdrawal that mimic OCD symptoms
Substance use disorder
Alcohol Withdrawal: Seizures and Delirium Tremens (DTs
Alcohol Withdrawal
Understanding the timeline and symptoms is essential for effective management
Happens With Heavy drinkers who stop drinking alcohol abruptly
Onset.. 6 to 24 hours after the last drink
Clinical features signs and Symptoms
Tremor
Anxiety
Headache
Palpitation
Sweating
GI upset
Mental status intact
Indicates that the patient is early on in the Withdrawal state
Alcohol Withdrawal Seizures
Timing and Incidence
High risk between 6 to 48 hours of Last Drink
Peak incidence occurs around 24 hours after cessation or reduction of alcohol use
Approximately 25 to 33% of patients with significant withdrawal experience seizures
Types of Seizures
Typically generalized tonic clonic or partial seizures
Single or in clusters of 2 to 3
Progression to DTs
About 30 to 50% of patients who experience seizures may progress to Delirium Tremens
Alcohol hallucinosis
Occurrs between 12 to 48 hours of Last Drink
Visual hallucinations
Seeing insects or animals
Auditory hallucination
Hearing voices
Tactile sensation
Feel like bugs crawling on skin
Delirium Tremens DTs
Neurobiology of DTs
Chronic alcohol exposure leads to
1. Upregulation of NMDA glutamatergic receptors
2. Downregulation of GABA receptors
3. Increased central norepinephrine activity
Cessation of alcohol results in CNS hyperactivity due to the lack of opposition to excitatory states
Onset and Duration
DTs usually begin 72 to 96 hours. 3 to 4 days. after cessation of alcohol/// but can appear up to 10 days later
90% of cases occur within 7 days following the last drink
Until then should be kept under observation
Nature and Severity
DTs is classified as a medical emergency with a mortality rate of up to 20% if untreated
Symptoms of DTs
Hyperactive Delirium with Psychosis
Altered Mental Status Features include altered consciousness,
1. hyperalertness,
Agitation
2. fear
3. suggestibility
Hallucinations Vivid visual, auditory, and tactile hallucinations
Autonomic Hyperactivity Symptoms include
1. tachycardia,
2. hypertension,
3. fever,
4. diaphoresis,
Drenching sweats
5. mydriasis pupillary dilation
Motor/Neurological Symptoms Increased hand tremors, psychomotor agitation, and ataxia
Treatment of Alcohol Withdrawal
Supportive Care
Importance of hydration and cautious use of neuroleptics and restraints
The patient can possibly die because of
Arrhythmia
Hyperthermia
Electrolyte and fluid abnormality
Thiamine Administration
Essential to administer thiamine 100 mg IM/IV before glucose to prevent Wernicke's encephalopathy
Lookout for //// Wernicke's encephalopathy can be precipitated by glucose in thiamine deficient states
Symptom triggered therapy
CIWA Scale
Clinical Institute Withdrawal Assessment for Alcohol Every four to six hours
Give Benzodiazepine if the score is High
Benzodiazepines
Primary treatment for both alcohol withdrawal seizures and DTs
Used for
Treating and preventing seizures
Preventing and managing symptoms of DTs eg by, lorazepam IV bolus
Preference for "Out The Liver" benzodiazepines
Oxazepam, temazepam, and lorazepam are preferred in patients with hepatic impairment due to their metabolism
Usually during the First week
Treatment Reduce the risk of relapse After the initial Symptom management
FDA approved drugs
Disulfiram
Naltrexone
Acamprosate
Support group
Alcohol Anonymous
Dx Criterion
DSM5
Two or more during 12 months
1. Tolerance
2. Withdrawal
3. Unable to Control use
4. Waste a lot of time to obtain/ use/ recover
5. Craving
6. Social occupational decline
Psychology correlate
Stages of change [5]
PC PAM
Psychological stages of change when trying to quit substance abuse
Pre contemplation
Does not acknowledge the problem
The damage they're doing to their body
No intention to change the behavior
Contemplation
Awareness the problem exists
Not willing to change
Preparation
Intention to change/ take action
Will usually have a reason for example I want to quit drinking because of my children
Action
Maintenance
Relapse
Alcohol
Metabolized in the Liver
Alcoholic Beverages
Mechanism of action
CNS Depressant
Intoxication clinical features
Slur speech
Incoordination
Stupor
Coma
Alcohol intoxication
Diagnosis
Serum blood alcohol concentration
Very high BAC levels
Alcohol poisoning
Respiratory depression can be fatal and requires ICU care
Legal limit for driving US
80 mg per deciliter
Number of drinks to achieve this BAC varies with size
Biomarker used to detect liars
Chronic use of alcohol causes increased MCV nd Resistant HTN
Neurocognitive decline
Basal Ganglia Disorders
Huntington's Disease
Autosomal dominant chromosomal disease (CAG trinucleotide repeats on chromosome 4).
Typically presents in middle age with movement disorder (chorea) and subcortical dementia.
Prone to mood disorders.
Anticipation is a key feature.
Imaging: atrophy of the caudate nucleus leading to "bat-wing" ventricles (anterior horns of lateral ventricles bowed outward).
Encephalitis & Prion Syndromes
Creutzfeldt-Jakob Disease (CJD)
Rapidly progressive spongiform encephalopathy (prion disease).
Features: rapidly progressing dementia, exaggerated startle response, violent unprovoked myoclonus.
EEG: periodic sharp-wave complexes.
CSF: elevated 14-3-3 protein kinase inhibitor and tau protein.
Other human prion diseases: Kuru, Gerstmann-Straussler-Scheinker (GSS) disease, Fatal Familial Insomnia (FFI).
Prion Disease eg, CreutzfeldtJakob Disease
CJD Insidious onset and rapid progression Motor features myoclonus, ataxia MCQ Point Fast polyphasic waves on EEG and CSF 1433 protein assay are supportive Always fatal, no accepted treatment
Cortical/Localization Syndromes
Balint's Syndrome
Triad: simultanagnosia (inability to attend to more than one visual item), optic ataxia (inability to guide reaching despite adequate vision), oculomotor apraxia (inability to voluntarily direct saccades).
Due to bilateral superior-parieto-occipital region damage.
Gerstmann Syndrome
Tetrad: dysgraphia/agraphia, dyscalculia/acalculia, finger agnosia, right-left disorientation.
Associated with dominant parietal lobe lesions.
Anton's Syndrome
Blindness with anosognosia (patient denies blindness and confabulates).
Classically associated with bilateral occipital cortex lesions.
Infectious
Neurosyphilis
Herpes Simplex Encephalitis
Affects temporal lobes, often resulting in residual amnesia.
Can cause Klüver-Bucy Syndrome (bilateral medial temporal lobe dysfunction affecting amygdala, leading to hyperorality, hypersexuality, docility, visual agnosia).
HIV
Subacute Sclerosing Panencephalitis (SSPE)
Late complication of measles virus infection.
Features: personality/cognitive changes, myoclonic seizures, spasticity, choreoathetoid movements, dysphagia, leading to coma and death.
Dementia Syndromes
Alzheimer's Disease (AD)
Pathophysiology: diffuse global atrophy.
Genetic risk: Apolipoprotein E (ApoE) E4 allele is the strongest genetic risk factor for late-onset AD.
Neurotransmitter: depletion of muscarinic receptors in cerebral cortex.
Dementia with Lewy Bodies (DLB)
Core features: fluctuating cognition, recurrent visual hallucinations, and parkinsonism.
Suggestive features: REM sleep behavior disorder, severe neuroleptic sensitivity.
Pathology: intraneuronal alpha-synuclein aggregates (Lewy bodies).
Frontotemporal Dementia (FTD) / Pick's Disease
Early changes in personality and behavior are characteristic, with primitive reflexes present.
Imaging: preferential atrophy of frontal and temporal lobes.
Pathology: Pick inclusion bodies.
Vascular Neurocognitive Disorder (VND) / Binswanger's Disease
Small infarctions of the white matter that spare the cortical grey matter.
Associated with lacunar infarcts.
Normal Pressure Hydrocephalus (NPH) / Hakim-Adams Syndrome
Triad: dementia, gait apraxia, urinary incontinence.
CSF accumulation in ventricles without significant rise in intracranial pressure; often reversible with shunting if identified early.
Metabolic (Reversible causes)
eg, Vitamin B12 deficiency
Wernicke's Encephalopathy Diagnostic Approach
Core Diagnostic Principle
Clinical Diagnosis First
Primarily a clinical diagnosis
High index of suspicion essential
Classic triad present in 10% of cases
Treatment with parenteral thiamine should be empirical
Glucose before thiamine can worsen condition
Neuroimaging
Magnetic Resonance Imaging MRI
Most valuable diagnostic tool
High specificity 93%), moderate sensitivity 53%
Characteristic findings on T2weighted, FLAIR, DWI
Key regions affected
Mammillary bodies
Thalamus
Periaqueductal gray matter
Third and fourth ventricles
Midbrain tegmentum/colliculi
Hypothalamus
Mammillothalamic tract
Practical tip Request coronal sections through mammillary bodies
Computed Tomography CT Scan
Can identify lowdensity abnormalities
May be normal in WE
Less sensitive than MRI
Wernicke's Encephalopathy Overview
Clinical Features
Thiamine Vitamin B1 deficiency
Classic Triad
Encephalopathy delirium or confusion
Gait Ataxia widebased gait
Oculomotor Dysfunction nystagmus, ophthalmoplegia
Aetiology & Prevalence
Rare under 35 years old
Common in chronic alcoholics, malabsorption, systemic malignancy
Additional Signs
Vestibular dysfunction
Peripheral neuropathy
Hypothermia
Cardiac involvement heart failure
Diagnostic Challenges
Often undiagnosed in 80% of cases
Can present as partial syndrome
Pathological Findings
Atrophy and discoloration of mammillary bodies
Capillary proliferation, gliosis, neuronal loss
Laboratory Investigations
Thiamine Levels
May be unreliable and delayed
Do not delay treatment for results
Erythrocyte Transketolase Activity
Decrease indicates potential WE
Nonroutine and not readily available
Plasma Pyruvate
Increase can indicate WE
Nonroutine and not typically available
Other General Blood Tests
Magnesium levels
Albumin levels
Complete Blood Count CBC
Comprehensive Metabolic Panel CMP
Management
Immediate Thiamine Administration
Dosage 100 mg IV or IM
Order thiamine before glucose
Followup 50100 mg IV 5 times a day
Magnesium Sulphate
Administer 24 grams IV bolus, then 14 grams IV every 4 hours
Prognosis & Reversibility
Generally reversible with treatment
Improvement in delirium, gait, eye movements
Residual deficits 40% ataxia recovery, 20% amnesia recovery
Korsakoff's Syndrome Sequela
Impaired shortterm memory, confabulation
Chronic condition with 20% recovery rate
Differential Diagnosis
Normal Pressure Hydrocephalus NPH
Neurocognitive disorder, gait ataxia, urinary incontinence
No ophthalmoplegia
. Amnestic Syndromes
Wernicke-Korsakoff Syndrome
Wernicke's Encephalopathy: Acute neurological emergency due to thiamine deficiency (Vit B1), especially in alcohol abusers.
Classic triad: ophthalmoplegia, ataxia, confusion.
Korsakoff's Syndrome (Amnesic Syndrome): Chronic amnesia, characterized by severe anterograde amnesia (difficulty learning new information), confabulation.
Develops in ~80% of patients recovering from Wernicke's encephalopathy.
Lesions in dorsomedial thalamus, mammillary bodies.
Thyroid disease
Hepatic encephalopathy
Thyroid disease
Irreversible
Wilson's disease
Neurodegenerative
Alzheimer's Disease
AD Most common cause 66% Cortical deficits 4As amnesia, aphasia, agnosia, apraxia Often presents with memory and learning decline
Lewy Body Disease LBD
Second most common 20% Key features fluctuating cognition, recurrent detailed visual hallucinations, Parkinson motor symptoms starting after cognitive decline MCQ Point Severe neuroleptic sensitivity is a suggestive feature therefore antipsychotics should be avoided if possible
Vascular NCD
Third most common 15% Onset temporally related to cerebrovascular events Prominent decline in complex attention and frontalexecutive function Often has a stepwise progression Emotional incontinence pseudobulbar affect is common Control of vascular risk factors can improve cognition
Frontotemporal Lobar Degeneration FTLD
Often presents with disinhibition, apathy, dysexecutive syndrome, aphasia
Huntington's Disease Neurologic
Demyelinating & White Matter Syndromes
Central Pontine Myelinolysis (CPM) / Osmotic Demyelination Syndrome
Caused by rapid correction of hyponatremia.
Demyelination can affect cerebrum and other CNS areas, not just pons.
Marchiafava-Bignami Disease
Rare disorder of demyelination and necrosis of the corpus callosum.
Strongly associated with chronic alcohol (particularly red wine) abuse.
Causes dementia.
Multiple Sclerosis (MS)
Common inflammatory demyelinating disease.
Psychiatric symptoms are common: depression (most common, e.g., due to interferon-beta), mania, pathological laughing/crying (pseudobulbar affect), emotional lability.
Neurological signs: fatigue (~75%), internuclear ophthalmoplegia (MLF lesion), Uhthoff's phenomenon (heat sensitivity), Lhermitte's sign (electric shock down spine with neck flexion).
Concordance rate in monozygotic twins: ~25-30%.
AI against NMJ
Myasthenia Gravis
Autoimmune disorder characterized by antibodies against nicotinic acetylcholine receptors at the neuromuscular junction.
Other Neurological Syndromes
Miller-Fisher Syndrome
Classic triad: gait ataxia, areflexia, ophthalmoplegia.
Restless Leg Syndrome (RLS) / Ekbom's Syndrome - Repeated here for emphasis in movement category.
Traumatic Brain Injury TBI NCD
presents immediately after TBI or once consciousness recovered, then persists
Hematoma
Subdural
epidural
Wilson's Disease Diagnostic Criteria and Lab Investigations
Overview of Wilson's Disease
Autosomal recessive disorder
Defect in copper transporter gene on chromosome 13
Copper accumulation in brain, liver, and other tissues
Clinical Features
Onset
Typically before age 40
Can begin as early as 3 years old
Neurological Symptoms
Parkinsonism
Bradykinesia
Rigidity
Dysarthria
Slurred speech
Gait changes
Clumsy, ataxic
Tremor
Dystonia
Involuntary movements
Cognitive decline and dementia
Psychiatric Symptoms
Psychosis
Mood lability
Depression
Anxiety
Ocular Signs
KayserFleischer rings
Copper deposits around the iris
Hepatic Manifestations
Hepatic cirrhosis
Enlarged liver
Sign for metabolic disorder
Lab Investigations
Diagnosis confirmation
Specific laboratory and clinical findings
Slitlamp examination
Detect KayserFleischer rings
Copper deposits on the cornea
Serum ceruloplasmin levels
Typically low
24hour urine copper levels
Typically high
MCQ Tips
Triad of symptoms
Neurological
Psychiatric
Hepatic
Key lab findings
Low ceruloplasmin
High urine copper
Classification of NCD
protein aggregate
Synuclein
Lewy Body Dimentia
alpha synuclein gen brain deposit
cognitive then motor symptoms
visual association cortex overactive
visual hallucination
Neuroleptic Hypersensitivity
no DA antagonist
ach recep post syn
basal forebrain nuc of mynert
Cant give Anticholinergic
N
Parkinsons Disease
Amyloid
Alzheimers
Amyloid beta (Aβ) insoluble form: Aβ-42
Low levels of Amyloidβ42 are a biomarker of amyloid deposition
Senile (Neuritic) Plaques
Early-Onset
Presenilin 1 (PSEN1 on chr 14), Presenilin 2 (PSEN2 on chr 1)
Late-Onset AD
is a risk-conferring allele
Apolipoprotein E (ApoE) epsilon 4 (ε4) allele
ApoE is involved in clearing cholesterol and Amyloid-β from the brain
allele is protective
ApoE epsilon 2 (ε2) allele
tau in ach prod
Tau
Down Syndrome
Picks
Alzheimers
Ch Traumatic Encepahalopathy
Prion
normally Found throughout the body and brain, folded into a helical shape, involved in communication, transport, and memory
vs Infectious Prions
Misfolded into a flat sheet structure, lose their function, and crucially, induce other normal prion molecules to misfold
General Management Principles for NCD
Identify and Treat Underlying Causes/Contributors This is crucial
Medications Contributing to Cognitive Impairment/Delirium Alcohol, analgesics NSAIDs, opioids, anticholinergics, antihistamines, hypnotics, benzodiazepines, H2 blockers, antispasmodics, anticonvulsants
Management of Agitation and Psychosis
Firstline Nonpharmacological interventions eg, "nofail" environment, optimal stimulation, sleep hygiene, sensory correction, reassurance, occupational therapy, caregiver education
Pharmacological Reserve antipsychotics for severe, dangerous, or distressing symptoms that have not responded to nonpharmacologic measures
Antipsychotic Use Start low doses, monitor monthly, discontinue in 4 weeks if ineffective/intolerable Haloperidol and injectables are NOT firstline
MCQ Point Antipsychotics carry a boxed warning for increased mortality in elderly patients with dementiarelated psychosis
General Diagnostic Criteria 🧠
Exclusions Not exclusively during delirium, not better explained by another mental disorder
Level of Diagnostic Certainty & Specifiers
Certainty "Probable" or "Possible" regarding etiology, with specific criteria for each
Specifiers
With or without behavioral disturbance eg, psychotic symptoms, mood disturbance, agitation
Severity Mild, Moderate, Severe applies to Major NCD only
Severity
Major NCD Significant cognitive decline in ≥1 domain, interferes with independence in daily activities
MCQ Point The primary discriminator between Major and Mild NCD is interference with independence in daily activities
Mild NCD Modest cognitive decline, does not interfere with independence, but may require compensatory strategies
Diagnostic Assessment 🔍
Step 1 Diagnose Clinical Presentation
History subjective complaints, functional dysfunction, neuropsychiatric symptoms
Objective assessment of cognitive deficits eg, MiniCog screen, neuropsychological testing Neuropsychological testing is preferably documented but not required in routine NCD assessments
Step 2 Establish Etiology
Physical and neurological examination
Required Laboratory Tests Complete CBC, Electrolytes, Glucose, BUN/Creatinine, TSH, Liver enzymes, Vitamin B12, Urinalysis
Structural Neuroimaging MRI/CT Always order to rule out treatable etiologies eg, neoplasm, stroke, subdural/epidural hematoma, hydrocephalus, CO poisoning
Not Routine Labs/Tests Order with specific indication Urine drug screen, Syphilis/HIV serology, Functional neuroimaging SPECT/PET, EEG, Lumbar puncture, DNA analysis, Biomarkers
MCQ Point "From 100, subtract 7" assesses calculation and sustained attention
Types
cortical
sub cortical
mixed
Aphasia
Primary Progressive Aphasia
Prog decline NCD Primarily Language over 2 years
writing
naming
word find
Reading
Preserved SAMPLE
Associated with FTD and Alzheimers
Fluent
Conduction Aphasia
Clinical Features
Comprehension intact
Repetition NA
Naming NA
Pathology.. Speech Production due to damage to Arcurate Fasiculus which interconnects Wernicke and Brocas area
Wernicke
DD Mania
Area involved
sup temporal gyrus
Clinical Features
Receptive
Nonsense content, Paraphasia ( meaningless ) and Neologism
Associated Deficit R Sensory loss and Right Visual Field cut
Non fluent
Anomic
GreStman Syndrome .
Clinical Features
Word finding difficulty
Frequent pauses and circumlocutions
Comprehension intact
Repetition intact
area damaged is angular gyrus
Global Aphasia
Clinical Features
Fluency NA
Comprehension NA
Repetition NA
Pt Mute utter only un intelligent sound
Broca
DD Psychotic withdrawal
area
44 left anterior frontal
clinical features
Expressive
Effortful
Laborious
frequent pauses
Telegraphic
Repetition impaired
naming impaired
awareness intact which leads to frustration
Associated Hemiparesis
Eating disorder
Bulimia Nervosa (BN
I Definition and Core Features
A Recurrent Episodes of Binge Eating
1 Amount Larger food quantity in 2hour period
2 Control Lack of control during episodes
B Recurrent Inappropriate Compensatory Behaviors
1 Selfinduced vomiting most common
2 Misuse of laxatives, diuretics, medications
3 Fasting
4 Excessive exercise
C Frequency and Duration
1 At least once a week for 3 months
D Selfevaluation Influenced by Body Shape and Weight
E Disturbance Not Exclusively During Anorexia Nervosa Episodes
II Epidemiology
A Gender
1 More common in females approx 101 ratio
B Age of Onset
1 Begins in adolescence or young adulthood 16–19 years
C Prevalence
1 Approximately 1–3% of young women
III Aetiology / Risk Factors
A Biological Factors
1 Genetics 4 times higher risk for relatives
2 Neurochemistry Serotonin, noradrenaline, plasma endorphins
3 Brain Structure/Function Increased grey matter in medial orbitofrontal cortex
B Psychological Factors
1 History of dieting behavior
2 Low selfesteem
3 Poor impulse control
4 Negative mood as a binge trigger
5 Perfectionism less significant than in AN
C Sociocultural Factors
1 Western cultural pressure to be slim
2 Peer influence
3 Adverse childhood experiences
IV Clinical Presentation and Symptoms
A Weight
1 Typically normal weight or overweight
B Physical Signs
1 Dental decay/erosion
2 Parotid gland enlargement Sialadenosis
3 Russell’s sign calluses on hands
4 Chronic sore throat, hoarseness
5 Weakness and dizziness
C Gastrointestinal Symptoms
1 Abdominal pain, bloating, constipation
2 Acid reflux, ulcers, esophagitis
D Electrolyte Abnormalities
2 Urinary chloride low in metabolic alkalosis
1 Hypokalemia, hypochloremia, metabolic alkalosis
E Other Laboratory Abnormalities
1 Elevated serum amylase
2 Increased pancreatic enzymes
F Menstrual Irregularity/Amenorrhoea
G Emotional/Cognitive
1 Intense guilt, shame, low selfesteem
H Covert Nature of Bingeing and Purging
V Differential Diagnosis
A Anorexia Nervosa AN
1 Key Differentiator BN patients maintain normal/overweight BMI
B Binge Eating Disorder BED
1 Key Differentiator BED has no compensatory behaviors
C Avoidant/Restrictive Food Intake Disorder ARFID
1 No preoccupation with body image
D Rumination Disorder
1 Repeated regurgitation of food, no fear of weight gain
E Other Specified Feeding or Eating Disorder OSFED
1 Criteria for specific eating disorder not fully met
F Unspecified Feeding or Eating Disorder
1 Insufficient data for definitive diagnosis
G Medical Conditions
1 Conditions causing vomiting without body image concerns
H Psychiatric Comorbidities
1 Depressive and Anxiety Disorders
2 Substance Use Disorders SUD
3 Borderline Personality Disorder BPD
VI Complications
A Medical Complications
1 Electrolyte disturbances hypokalemia, metabolic alkalosis
2 Cardiac issues arrhythmias, heart failure
3 Gastrointestinal damage esophageal tears, ulcers
4 Seizures due to electrolyte imbalance
5 Dehydration
6 Osteoporosis
B Psychiatric Complications
1 High comorbidity with depression and anxiety disorders
2 Elevated suicide risk 2533% report suicidal ideation
VII Prognosis and Course
A Variable course chronic or intermittent
B Better prognosis than anorexia nervosa
C 50–75% achieve full recovery or substantial improvement
D Relapse risk about onethird within 4 years
E Poor prognostic factors long duration, severe symptoms, comorbidity
VIII Management
A Psychotherapy FirstLine
1 Cognitive Behavioral Therapy CBTBN
2 Other therapeutic approaches may be considered
B Pharmacotherapy
1 FDA approved medications for BN
2 Consideration of comorbid psychiatric conditions
Rumination Disorder
I Definition & Core Features
A Definition
1 Characterized by repeated regurgitation of food over at least 1 month
B Mechanism
1 Occurs via retrograde peristalsis or contraction of abdominal wall muscles
C Regurgitated Food
1 May be rechewed, reswallowed, or spit out
D Nature of Regurgitation
1 Effortless and painless
2 Occurs soon after a meal within minutes to an hour
3 Frequent several times per week, typically daily
4 Volitional but described as habitual or outside control
II Diagnostic Criteria DSM5 / DSM5TR
A Repeated regurgitation of food for at least 1 month
B Not attributable to gastrointestinal or other medical conditions
1 Rule out conditions like gastroesophageal reflux, pyloric stenosis
C Does not occur exclusively during other eating disorders
1 Anorexia Nervosa, Bulimia Nervosa, BingeEating Disorder, Avoidant/Restrictive Food Intake Disorder
D Symptoms in the context of another mental disorder must warrant additional clinical attention
E Specify if in remission
III Associated Features
A Infants
1 Straining and arching of the back, sucking movements
2 May gain satisfaction from activity, can be irritable and hungry
3 Rumination may serve selfsoothing or selfstimulatory function
B Older children/Adults
1 May disguise behavior hand over mouth, coughing
2 Avoid eating with others due to embarrassment
3 Common feelings of shame and embarrassment
C Medical Consequences
1 Weight loss and failure to gain expected weight common in infants
2 Severe malnutrition
3 Gastrointestinal issues abdominal pain, bloating, constipation, nausea, diarrhea
4 Dental problems/decay
5 Halitosis
6 Aspiration, recurrent respiratory tract infections, asphyxiation rare but can be fatal
IV Prevalence & Epidemiology
A Historically described in individuals with intellectual disability
B Occurs in adults with normal intelligence
C Approx 12% of gradeschoolage children
D More common among male infants similar rates in boys and girls aged 1016 in Sri Lanka
E Rare in older children and adolescents
V Development & Course
A Onset
1 Can occur in infancy, childhood, adolescence, or adulthood
2 Infants usually between 3 and 12 months
3 Older children/adolescents mean age of onset around 15 years
B Course
1 Can be episodic or continuous
C Remission
1 Frequently remits spontaneously, especially in infants
2 Can persist throughout life
VI Risk & Prognostic Factors
A Risk Factors
1 Intellectual disabilities
2 High anxiety or stressful/neglectful environments
3 Problems in parentchild relationship
4 Overstimulation and tension
5 Gastroesophageal reflux or acute illness may precede onset
B Prognosis
1 High rate of spontaneous remission
2 Behavioral interventions eg, habitreversal techniques improve prognosis
VII Differential Diagnosis
A Distinguish from gastrointestinal or other medical conditions
1 Gastroparesis, pyloric stenosis, hiatal hernia, Sandifer syndrome
B Other Eating Disorders
1 Anorexia Nervosa, Bulimia Nervosa, BingeEating Disorder, Avoidant/Restrictive Food Intake Disorder
2 Rumination disorder cannot be diagnosed exclusively during their course
C Major Depressive Disorder
1 Rumination in MDD is moodcongruent, not necessarily intrusive
D ObsessiveCompulsive Disorder OCD
1 Rumination involves repetitive, unpleasant thoughts linked to compulsions
E Generalized Anxiety Disorder GAD
1 Excessive worry about reallife concerns without compulsions
F Schizophrenia
1 Ruminative delusional thoughts with other characteristic symptoms
VIII Comorbidity
A Can occur with intellectual disabilities
B May occur with anxiety disorders, especially severe ones
C Can be diagnosed with other psychiatric conditions eg, autism spectrum disorder, schizophrenia
D Can be comorbid with other eating disorders
IX Treatment
A Firstline
1 Diaphragmatic breathing most effective behavioral intervention
B Behavioral Interventions
1 Habitreversal techniques eg, chewing gum
2 Aversive behavioral interventions eg, squirting lemon juice
C Education
1 For patient and parents/caregivers regarding motherchild relationship deficits
D Medication
1 Not standard part of treatment
2 Some medications metoclopramide, cimetidine, haloperidol cited as helpful
3 Pharmacologic treatment for comorbid anxiety and depressive symptoms may be included
4 Baclofen and TCAs studied but show no significant evidence of benefit
Preparing for a MCQ Based Exam on Anorexia Nervosa Complications
Complications Overview
Hormonal Complications
Hypogonadism
Low levels of FollicleStimulating Hormone FSH and Luteinising Hormone LH
Results in low estrogen/testosterone levels
Amenorrhoea
Cessation of menstrual periods in females
Leptin Deficiency
Low leptin levels affecting appetite control
Hypothyroidism
Reduced thyroid function leading to metabolic issues
Hypercortisolaemia
Elevated cortisol levels indicating stress response
Biochemical/Metabolic Disturbances
Electrolyte Imbalances
Lifethreatening conditions like
Hypokalaemia
Hypocalcaemia
Hypophosphataemia
Hypomagnesaemia
AcidBase Disturbances
Metabolic Acidosis
Common with laxative abuse
Metabolic Alkalosis
Common with vomiting
Nutritional Deficiencies
Thiamine B1, Vitamin B12, Iron deficiencies
Liver Enzyme Elevations
Transaminitis
Key Points for MCQs
Highest Mortality Rate
Anorexia nervosa has the highest mortality rate of any psychiatric disorder
Refeeding Syndrome
Critical risk during weight restoration
Characterized by hypophosphatemia, hypokalemia, hypomagnesemia
Lab Workup Priority
Initial medical evaluation must include electrolytes and EKG
Hormonal Complications in Detail
HypothalamicPituitaryGonadal HPG Axis Dysfunction
Amenorrhea
Absence of menstrual cycles
Can precede weight loss
Decreased Sex Hormones
Low estrogen and testosterone levels
Thyroid Dysfunction
Sick Euthyroid Syndrome
Mild hypothyroidism with low T3
Adrenal Axis Dysfunction
Raised Cortisol Levels
Increased cortisol as an adaptive mechanism
Growth Hormone Regulation Issues
Raised Growth Hormone Levels
Impact on bone mass and growth
Insulin and Leptin
Abnormal Insulin Secretion
Decreased insulin and leptin levels
Biochemical Complications in Detail
Electrolyte Imbalances
Commonly observed
Hypokalemia
Hyponatremia
Hypochloremia
Hypophosphatemia
Hypomagnesemia
Hypocalcemia
AcidBase Disturbances
Metabolic Alkalosis
Common with selfinduced vomiting
Metabolic Acidosis
Associated with laxative abuse
Lipid Profile
Hypercholesterolemia
One of the few elevated lab values
Liver Enzymes
Elevated Hepatic Enzyme Levels
Common during refeeding
Renal Markers
Elevated Blood Urea Nitrogen BUN
Reflects dehydration
Hematological Abnormalities
Leukopenia, Mild Anemia, Thrombocytopenia
Glucose Metabolism
Hypoglycemia
Rare but poor prognostic indicator
Vitamins and Minerals
Vitamin D, Zinc, Thiamine deficiencies
Amylase
Elevated Serum Amylase
Often due to vomiting
Refeeding Syndrome A Critical Complication
Definition
Potentially fatal disruption in electrolytes during renourishment
Hallmark Biochemical Abnormality
Profound Hypophosphatemia
Mechanism involves insulin release and cellular uptake
Other Key Electrolyte Disturbances
Hypokalemia and Hypomagnesemia
Vitamin Deficiency
Thiamine deficiency leading to Wernicke's encephalopathy
Clinical Features
Muscle weakness, seizures, cardiac dysrhythmias
Prevention
Initiate nutritional support slowly, monitor electrolytes carefully
Anorexia nervosa
Complication
Refeeding Syndrome A Critical Complication
Definition
Definition nnd Occurrence
Refeeding syndrome occurs when the nutritional state of a starved or malnourished person is restored too rapidly 🥗
It refers to severe electrolyte and fluid shifts associated with metabolic abnormalities during renutrition
Typically occurs within the first few days of renutrition
Can be fatal if not managed properly
Pathophysiology The "Why"
Insulin Release
Renutrition, especially with carbohydrates a glucose load, stimulates insulin release 🍞
Cellular Uptake
Insulin activates protein, fat, and glycogen synthesis
Requires a rapid shift of electrolytes phosphate, magnesium, potassium and water into the cells from the bloodstream
Fluid Imbalance
Fluid retention and edema, particularly peripheral edema
Metabolic Shift
Change from fat to carbohydratebased energy production
Potentially fatal disruption in electrolytes during renourishment
Hallmark Biochemical Abnormality
Profound Hypophosphatemia
Mechanism involves insulin release and cellular uptake
Leads to a deficit in adenosine triphosphate ATP
Elevated Hepatic Enzyme Levels
Other Key Electrolyte Disturbances
Hypokalemia and Hypomagnesemia
Vitamin Deficiency
Thiamine deficiency leading to Wernicke's encephalopathy
Thiamine B1, Vitamin B12, Iron deficiencies
Anemia
B1
Thiamine Deficiency
Increased cellular utilization of thiamine in response to carbohydrate refeeding
Can precipitate Wernicke’s encephalopathy if not prevented by supplementation
Clinical Features
Muscle weakness, seizures, cardiac dysrhythmias
Prevention
Initiate nutritional support slowly, monitor electrolytes carefully
Pic monic
Angry heart
Angry Liver
dEC PKM
Banana
Current seizure
Low weight weak muscles
Eating a lot of food
She REfeedIN
Neurological Symptoms
Symptoms include delirium, seizures, confusion, muscle weakness, myoclonus, and mild neuropathies
Risk Factors Who's at risk?
Malnutrition
Severely malnourished individuals are at the highest risk 🍽️
Low Body Weight
BMI < 16 kg/m², <70% ideal body weight, or significantly low body weight for height, age, and developmental stage
Prolonged Poor Intake
Little to no nutritional intake for 10 days prior to admission, or underfed for at least 10–14 days
Recent Significant Weight Loss
Weight loss of >10% in the last 1–2 months increases risk
Abnormal Electrolytes at Presentation
Indicates existing depletion and increases susceptibility
Specific Conditions
Patients with eating disorders especially anorexia nervosa and alcoholism are particularly vulnerable
Often missed in psychiatric units
Management and Prevention The "How to fix/avoid"
Slow Refeeding Gradual Renourishment
Cornerstone of prevention is to refeed slowly 🐢
Initial caloric intake should be low eg, 10-20 kcal/kg/day and increased gradually over days
Electrolyte Correction and Monitoring
Correct electrolyte abnormalities before refeeding begins
Close and frequent monitoring of electrolytes especially phosphate, potassium, magnesium is crucial, sometimes daily for the first week
Supplementation of phosphate, magnesium, and potassium as needed
Thiamine Supplementation
Prescribe thiamine and B vitamin complex/multivitamins with refeeding to prevent deficiencies
Fluid Management
Monitor and restrict fluid intake to prevent overload, especially in those at risk of cardiac dysfunction
Large boluses of IV fluids should be avoided to reduce risk
Medical Monitoring
Regular physical examinations, serial laboratory tests, and telemetry for cardiac symptoms are necessary
Setting of Care
Patients with severe nutritional compromise should be managed in an inpatient hospital setting
Appropriate specialty consultation dietitian, eating disorder psychiatrist, physician with expertise in nutrition is essential
Multidisciplinary Approach
Requires a multidisciplinary team to ensure comprehensive care
Prognosis
Potentially fatal, but preventable and treatable with appropriate management and monitoring
Hormonal Complications in Detail
HypothalamicPituitaryGonadal HPG Axis Dysfunction
Amenorrhea
Low levels of FollicleStimulating Hormone FSH and Luteinising Hormone LH
Decreased Sex Hormones
Low estrogen and testosterone levels
Absence of menstrual cycles
Cessation of menstrual periods in females
Can precede weight loss
Elevated cortisol levels indicating stress response
Hypercortisolaemia
Thyroid Dysfunction
Sick Euthyroid Syndrome
Mild hypothyroidism with low T3
Reduced thyroid function leading to metabolic issues
Adrenal Axis Dysfunction
Raised Cortisol Levels
Increased cortisol as an adaptive mechanism
Growth Hormone Regulation Issues
Raised Growth Hormone Levels
Impact on bone mass and growth
Insulin and Leptin
Abnormal Insulin Secretion
Decreased insulin and leptin levels
Low leptin levels affecting appetite control
Complications Overview
Biochemical/Metabolic Disturbances
Electrolyte Imbalances
Lifethreatening conditions like
Hypokalaemia
Hypocalcaemia
Hypophosphataemia
Hypomagnesaemia
AcidBase Disturbances
Metabolic Acidosis
Common with laxative abuse
Metabolic Alkalosis
Common with vomiting
Nutritional Deficiencies
Liver Enzyme Elevations
Transaminitis
Biochemical Complications in Detail
Electrolyte Imbalances
Commonly observed
Hypokalemia
Hyponatremia
Hypochloremia
Hypophosphatemia
Hypomagnesemia
Hypocalcemia
AcidBase Disturbances
Metabolic Alkalosis
Common with selfinduced vomiting
Elevated Serum Amylase
Often due to vomiting
Metabolic Acidosis
Associated with laxative abuse
Lipid Profile
Hypercholesterolemia
Liver Enzymes
Elevated Hepatic Enzyme Levels
Common during refeeding
Renal Markers
Elevated Blood Urea Nitrogen BUN
Reflects dehydration
Hematological Abnormalities
Leukopenia, Mild Anemia, Thrombocytopenia
Glucose Metabolism
Hypoglycemia
Rare but poor prognostic indicator
Vitamins and Minerals
Vitamin D, Zinc, Thiamine deficiencies
Osteoporosis/Osteopenia
for which physiologic oestradiol replacement may be considered
Cardiac Complications
Most common cause of death in refeeding syndrome
Includes arrhythmias,
heart failure including congestive heart failure, poor contractility, and low stroke volume ❤️
Amylase
Elevated Serum Amylase
Often due to vomiting
Key Points for MCQs
Highest Mortality Rate
Anorexia nervosa has the highest mortality rate of any psychiatric disorder
Refeeding Syndrome
Critical risk during weight restoration
Characterized by hypophosphatemia, hypokalemia, hypomagnesemia
Lab Workup Priority
Initial medical evaluation must include electrolytes and EKG
ey for MCQs: Remember that low leptin is a characteristic endocrine finding in Anorexia Nervosa
Neurodevelopmental
Neurotransmitters & Brain Pathways
A Reward System/Addiction
Nucleus accumbens as a key structure addictive drugs affect mesocorticolimbic pathways
B ADHD Neurochemistry
Norepinephrine increases signal dopamine decreases noise
C Tourette's Neurochemistry
Characterized by dopamine overactivity
D Olfactory Pathway
Does not relay through the thalamus
Intellectual Disability ID / Intellectual Developmental Disorder
Key Diagnostic Criteria
Onset During the Developmental Period
Identified during childhood or adolescence
Deficits in Intellectual Functions
Confirmed by both clinical assessment
Judgment and cognitive efficacy
hair judge
Reasoning,
R
abstract thinking
A
Planning,
P
problemsolving,
P
Verbal expression and comprehension
Verb Rap music
Working memory
W
learning from experiece
Exp star
and an individualized standardized test. Judge RAP2 W2
Deficits in Adaptive Functioning
Deficits in Adaptive Functioning
Failures to meet developmental and sociocultural standards
Primary measure of severity in DSM5
Areas of Adaptive Function
unmet developmental and sociocultural standards for personal independence
Self-care
Communication
Social/interpersonal skills
Work
Health
Safety
personal independence
Epidemology
gen pop
1%
Assoc
e Malform Synd
10%
e Genetic
35%
no1
Downs syndrome (trisomy 21):
no 1 Inherited
Fragile X syndrome
no 1 preventable
Fetal alcohol syndrome
IQ
IQ= {mental age / chrono age} x 100
stable throughout life
avq 90-110
Mean IQ = 100 [+/- 15]
classification
ID ≤ 70
Intellectual disability ≈ ≤ 70 or
2 standard deviation [SD=15] below the mean
Mild >50
IQ 50-55 to 70
(85% of total ID)
CFs
Social
Conceptual
Academic level: up to 6th grade
Practical
may need support with complex
need help in actions for eg.
Grocery shopping and meal preparation
money management
Health care and legal decisions
Moderate > 35
IQ 35-40 to 50-55
(10% of total)
CFs
Communication focuses on here and now
simple commands
Practical
requires support for all activities of daily living
Meal preparation, dressing, bathing,elimination
Severe > 20
IQ 20-25 to 35-40
CFs
And divided into three domains
Conceptual
Practical
dependent on others for ALL aspects of daily
1}physical care
2}health
3}safety
Require highly supervised setting
Social
very limited speech and communication
Express desires non-verbally / emotionally
Children under 5 fails to meet developmental milestones in several areas of intellectual function
severity level cannot be reliably clinical assessed or def tools due to (blindness, prelingual deafness)
Global Developmental Delay
Unspecified Intellectual Disability
For individuals over 5 years with difficult assessment
Assessment
of
IQ
infant
1–42 months
Bayley Scale for Infant & Toddler
Peabody Picture Vocabulary
Wechsler
WPPSI preschool
2.5y to 7.5y
14 subtests
Verbal IQ
through picture naming
Performance IQ
Processing speed
General language
Patient is shown a design and he has to copy it by manipulating the blocks
WISC
6-17 years
10 core subtests grouped into 4 indices
o Verbal comprehension o Perceptual reasoning o Working memory o Processing speed
Patient is shown a design and he has to copy it by manipulating the blocks
WAIS
non-verbal intelligence 4 speech or hearing impaired 2-20 y
Leiter
2-20 yrs
to
assess non-verbal intelligence
No need of spoken language during the test
for *
Who: cognitively delayed, disadvantaged, non-English speaking, hearing impaired, speech impaired, or autistic persons
Description
4 subtests
o Reasoning o Visualization o Memory o Attention
Peabody Picture Vocabulary Test (not for the def)
receptive vocabulary
Subject points to the picture most like the stimulus word spoken by examiner
175 picture plates with 4 pictures on each plate
Poor vocabulary is a hallmark of broader language, literacy, and cognitive difficulties
for
Who: verbally handicapped subjects But should not be def and intact hearing o Requires no reading or oral response o Hearing must be intact
adaptive function
Vineland Adaptive Behavior Scale
ID, developmental delay, ASD, ADHD
o Communication: receptive, expressive, written
follow instructions? no of steps?
identify objects in pic
understand touch ur elbow command
behavioral/psychiatric disturbances
General Principles
Definition of Neurodevelopmental Disorders
Conditions beginning early in development
Characterized by developmental deficits
Impairments in personal, social, academic, or occupational functioning
Tic Disorders
Tic Disorders
PANDAS Syndrome (Paediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal infections)
Autoimmune neurological disorder associated with OCD and tic disorder, exacerbated by beta haemolytic streptococcal infection.
Tourette disorder may be provoked by early repeated streptococcal infections.
Tourette's Disorder
Multiple motor and one or more vocal tics present for more than 12 months.
Requires both multiple motor tics and one or more vocal tics
Tics present for more than 1 year
Onset before age 18 years
Commonly comorbid with ADHD and OCD.
Family history of OCD is common.
Linked to dopaminergic neurons in caudate.
Persistent Chronic Motor or Vocal Tic Disorder
Requires either motor or vocal tics
Tics present for more than 1 year
Onset before age 18 years
Provisional Tic Disorder
Requires single or multiple motor and/or vocal tics
Tics present for less than 1 year
Onset before age 18 years
Attention Deficit Hyperactivity Disorder ADHD
Presentation Types
Predominately Inattentive Presentation
Predominately Hyperactive/Impulsive Presentation
Combined Presentation
Severity Specifiers
Mild, Moderate, Severe
Can be specified as "in partial remission"
Autism Spectrum Disorder ASD
DSM5 Changes
Combines previous Pervasive Developmental Disorders
Autistic Disorder, Asperger Syndrome, PDDNOS, etc
Reduced from three symptom categories to two core categories
SocialCommunication Impairment
Restricted, Repetitive Patterns of Behavior
Onset of symptoms in early developmental period
Specifiers
With or without intellectual impairment
With or without language impairment
Associated with known medical/genetic condition
Associated with another neurodevelopmental, mental, or behavioral disorder
With catatonia
Clinical features
Begin early in life and limit or impair everyday functioning
had significant language delays and a higher likelihood of intellectual disability
lifelong neurodevelopmental disorder
persistent deficits X in social communication and social interaction
RRBs I A
restricted, repetitive patterns of behaviour, interests, or activities
Asperger syndrome
milder form of autism with less severe symptoms and better functioning
had social difficulties but were able to live more independent lives
single gene = at DNA sequence within a gene.
FMR-1 gene (Fragile X Mental Retardation 1 gene)
Fragile X Syndrome
Most common inherited cause of mental retardation.
Caused by trinucleotide repeats (CGG) on Xq27.3.
Anticipation is seen (earlier onset, more severe symptoms in successive generations).
CF
face
long face, large ears,
prominent jaw, soft skin,
balls
large testicles (macroorchidism in postpubertal males)
Behavioral:
autistic-like features (shy, socially awkward, avoid eye contact, self-stimulatory, peculiar, self-injurious),
hyperactivity, higher rates of OCD, ADHD, dysthymia, anxiety, antisocial personality disorder.
autism in about 33% of cases
Associated with social anxiety disorder.
Mutation increases the number of CGG sequences on the DNA
Silenced the FMR-1 gene
methylation of its regulatory region
Fragile X mental retardation protein (FMRP)
involved in the development of synaptic connections
Also the most common identifiable etiology of autism
FMR-1 genetic test is recommended for all ASD work-ups
TSC1 (on 9q34) or TSC2 (on 16p13.3) genes
Tuberous Sclerosis Complex (TSC)
Known etiology of autism
Clinical triad: intellectual disability, seizures, and hamartomas (hypomelanotic macules/ash leaf spots and angiofibromas)
Seizures are common, especially infantile spasms
Vigabatrin is the treatment of choice
MECP2 gene on the X chromosome
Rett Syndrome
almost exclusively in females
X-linked dominant inheritance; seen almost exclusively in girls (male mutant foetuses typically do not survive).
Most often caused by mutations in the MECP2 gene (Xq28).
Characterized by developmental arrest and loss of milestones (after initial normal development), autistic-like features, mental retardation, stereotyped hand movements (e.g., hand wringing), spasticity, truncal ataxia, and apraxia.
Small hands and feet.
sporadic mutation during spermatogenesis, with only 1% being familial
Phenylketonuria (PKU
deficient hepatic enzyme, phenylalanine hydroxylase (PAH), which converts phenylalanine to tyrosine
leads to toxic levels of phenylalanine and phenyl ketone
musty odor
Genetics Deletion/mutation on maternal chromosome 15
Angelman Syndrome
Deletion in 15q12 of maternal origin.
Features: puppet-like movements, compulsive laughter, severe mental retardation, epilepsy.
Associated with microcephaly.
absence or non-functionality of several genes on the paternal chromosome 15 DUE TO genomic imprinting
Prader-Willi Syndrome
genomic imprinting
specific paternal genes are activated while maternal copies are silenced
absence or non-functionality of several genes on the paternal chromosome 15
clinical features
Features: obesity, small hands and feet, microorchidism/cryptorchidism (hypogonadism), short stature, almond-shaped eyes.
Behavioral: compulsive eating, skin picking, self-harm, OCD.
Self-talk is common.
CAG trinucleotide repeat expansion in the Huntingtin gene
Huntington's Disease
Deletion on chromosome 5p
Cri-du-Chat Syndrome
Copper transporter gene
Wilson's Disease
Congenital recessive condition of defective copper metabolism (chromosome 13).
Psychiatric symptoms (personality disturbances, mood abnormalities, cognitive dysfunction) are common and can be the first presentation.
Neuropathological finding: copper deposits in lenticular nuclei (pallidum and putamen) leading to brick red pigmentation in basal ganglia.
Kayser-Fleischer rings (copper deposits on Descemet's membrane of the cornea) are present in 95% of patients with neurological symptoms, and 50-60% without neurological symptoms.
23 Pairs of Chromosomes
Autosomes
first 22 pairs
Sex Chromosomes: The 23rd pair
determine an individual's biological sex
Y chromosome, specifically a gene on it called SRY (sex-determining region of Y),
In its absence, the individual develops as female
Neuroimaging Findings in Developmental Disorders
A ADHD Attention Deficit Hyperactivity Disorder
Smaller total cerebral, frontal lobe, caudate, cerebellar, and corpus callosal volumes
Lower prefrontal perfusion/metabolism and dopamine transporter levels
EEG shows increased slow wave activity in right prefrontal area
B Autism Spectrum Disorder ASD
Larger brain volume increased volumes in parietaltemporal lobes, cerebellum, corpus callosum, hippocampus, and amygdala
SPECT/PET reveals bitemporal and bifrontal hypoperfusion
C Reading Disorder Dyslexia
Size asymmetry difference in the planum temporale
D Tourette's Disorder
Larger right dorsolateral prefrontal cortex overactivity in prefrontal cortex and ventral striatum during tics
E Schizophrenia
Enlarged lateral ventricles significant brain changes if onset is before age 13
F Traumatic Brain Injury TBI
Diffusion Tensor Imaging DTI detects shear injuries
Brain Maturation & General Neurodevelopment
A Adult Brain Volume
Reached around 58 years of age
B Hemispheric Language Dominance
Establishes around 78 years
C Order of Maturation
Phylogenetically older regions mature first
1 Hippocampus and related structures
2 Primary motor and sensory cortex
3 Association cortices
4 Prefrontal Cortex Last to myelinate, continues into mid20s
D Myelination & Synaptic Pruning Adolescence
Myelination occurs around age 12, increasing signal speed
Synaptic pruning around age 12 "use it or lose it"
Substance Impact on Developing Brain
A Marijuana THC in Adolescence
Suppresses hippocampal neuron activity, affecting memory
Chronic exposure leads to neuron connection loss increases risk for adult psychosis in genetically vulnerable individuals
Early Neurological Assessment
A Neonatal Reflexes
Key reflexes Babinski sign, Doll’s eyes, Protective reflex, Rooting, Moro reflex
B Visual Functions at Birth
Black & white vision present color vision develops in the first week
Genetic Factors
A Fragile X Syndrome
Most common inherited cause of intellectual disability caused by CGG repeat expansion in FMR1 gene
Loss of Fragile X Mental Retardation Protein FMRP affects synaptic development
Most Common Genetic Cause of ID** | Down Syndrome (Trisomy 21) | | **Most Common Inherited Cause of ID** | Fragile X Syndrome | Single gene, X-linked dominant. | | **Most Common Preventable Cause of ID** | Fetal Alcohol Syndrome (FAS) | Environmental factor, often confused with genetic causes. | **Unknown Etiology** | Approximately 50% of all ID cases (Higher in mild ID, lower in severe ID). | Important baseline statistic.
NonHereditary Conditions
Mutation during gamete formation i.e meiosis non-disjunction
Down's Syndrome (Trisomy 21):
Down Syndrome (Trisomy 21)\ by an extra copy of chromosome 21.occurs during cell division in the formation of eggs or sperm. Non inherited
Overall the number1 Cause of Intellectual disability
pathology
caused by an extra copy of chromosome 21, hence also known as Trisomy 21 syndrome
3 mechanism of abnormal number of chromosomes (aneuploidy)
Full Trisomy 21 (Non-disjunction)
Results from nondisjunction during meiosis (failure of chromosomes to separate)
Risk Factor:
Strongly associated with advanced maternal age
Accounts for the overwhelming majority, around 92–95% of cases
Robertsonian Translocation:
Prevalence:
Accounts for 2–5% of cases
pathos
A fusion of two chromosomes, usually the extra chromosome 21 with another, typically chromosome 14 (also 13, 15, or 22)
Patients have 46 chromosomes but with extra 21 material attached to ch14
inheritance
Can be inherited from an unaffected parent (carrier). Carriers have 45 chromosomes
Recurrence Risk
The risk of having another child with Down Syndrome is highest if the first child has Robert translocation
Mosaic mix Down Syndrome
Milder features in mosaic Down syndrome.
Prevalence
Occurs in 1–2.5% of case
pathos
Nondisjunction occurs after fertilization in cell division, resulting in a mixture of normal and trisomic cells
Phenotype
Often results in a milder phenotype and less cognitive impairment, with IQ potentially in the 70s (compared to usually below 50 in full trisomy). Not associated with maternal age
Epidemiology [ Incidence & Risk Factors]
most common autosomal chromosomal disorder
no 1. genetic cause of learning disability (LD)
Incidence
1 in 700 to 1 in 1,000 live births
RISK Factor oo e DS3
Maternal age
Major risk factor: maternal age > 40 years.
The most important risk factor; risk increases significantly with maternal age, especially over 35 years
Father age
Increased risk with paternal age less than 20 or over 40 years
Previous Child:
Having a previous child with Down Syndrome increases the risk for subsequent pregnancies.
Clinical Features (Phenotype) [Characteristic Signs]
General Physical Features:
Characteristic features: epicanthic folds, flat nasal bridge, simian palmar crease, almond-shaped eyes.
Lax ligaments/hyperextensible joints
General hypotonia (reduced muscle tone),
incoordination
Short stature
Abundant neck skin (nuchal swelling)
Overweight/obesity (around 30% of cases)
characteristic FACE appearance
Oblique/upward-slanted palpebral fissures,
almond-shaped eyes
flat nasal bridge
Macroglossia
Iris white spots (Brushfield spots)
Microcephaly (small, flattened skull)
other physical complications OO e
45% have congenital heart disease (35-40% of these have AV septal defects).
Increased risk of hearing loss, hypothyroidism, leukaemia, obstructive sleep apnoea.
Associated with early-onset dementia in adulthood.
Edwards Syndrome (Trisomy 18)
Features: rocker bottom feet, low-set ears, micrognathia (small jaw), clenched hands, congenital heart disease, prominent occiput.
Severe intellectual disability.
chromosomal abnormalities
Patau Syndrome Trisomy 13
severe to profound intellectual disability
other Clinical features
severe organ malformations
severe renal, cardiac, and intestinal malformations
Features: overlapping of fingers over thumb.
Prognosis and survival
95% of affected individuals die in utero
Often death within 1 year of birth.
infants born alive, only about 5%-10% survive beyond one year of age
Mutation during gamete formation
Rett Syndrome
sporadic mutation during spermatogenesis, with only 1% being familial
pathology
caused by a mutation on the X chromosome in the MECP2 gene
Rett Syndrome X link
mutation during spermatogenesis
Clinical features
by a period of apparently normal early development
followed by a dramatic regression
and loss of previously acquired skills,
purposeful hand use, language, and mobility
almost exclusively in females
a period of normal development followed by deceleration of head growth, loss of purposeful hand skills (replaced by stereotyped hand movements), loss of social engagement, impaired language, and severe psychomotor retardation
Subtopic
-Deletion
-5p
Cri du Chat Syndrome
Partial deletion of 5p region (15.2).
Characteristic high-pitched, cat-like cry in infancy.
Features: pronounced microcephaly, round face with hypertelorism, epicanthic folds, slanting palpebral fissures, broad flat nose, low-set ears, micrognathia.
Behavioral: severe to profound mental retardation, hyperactivity, stereotypies, self-injury.
-22q
DiGeorge Syndrome (Velocardiofacial Syndrome - VCFS)
Microdeletion of chromosome 22q11.2.
(90%, 75% or more) arise de novo (sporadic)
10% are inherited, following an autosomal dominant pattern
Associated with learning disability and schizophrenia-like psychosis (25-30% develop schizophrenia).
COMT (Catechol-O-Methyltransferase), a reduction in which may contribute to psychosis
40% develop depression
Physical anomaly
CATCH 22 mnemonic: Cardiac defects, Abnormal facies, Thymic hypoplasia, Cleft palate, microdeletion of chromosome 22.
VSD), tetralogy of Fallot, interrupted aortic arch, and pulmonary atresia
microcephaly, long face, small mouth, prominent tubular or bulbous nose, small alae, micrognathia (small lower jaw), broad nasal bridge, minor ear abnormalities, and hypertelorism
complication
Hypocalcaemia: Present in 60% of patients due to hypoparathyroidism
Immune Deficiency: Due to thymic hypoplasia/aplasia
-7q
Williams Syndrome
microdeletion on chromosome 7q11.23
deletion on chromosome 17 Microdeletion on 17p11.2.
Smith-Magenis Syndrome
Features: bradydactyly, broad flat face, hoarse voice, characteristic fleshy upper lip.
Behavioral: prominent autistic features, hyperactivity (75%), inattention, severe self-injury (70%, e.g., head banging, nail pulling, hand biting), obsessive-compulsive behaviour, schizophrenia-like psychosis.
Sleep: reduced or absent REM phase.
somatic mosaic mutation in the GNAQ gene
Sturge-Weber Syndrome
overgrowth of blood vessels on the surface of the brain (leptomeningeal angioma
Port-Wine Birthmark
Occurs after Conception during Fetal development
Sex chromosome abnormalities
+
Klinefelter Syndrome (47 XXY)
47xxy or 48xxxy
Features: tall stature with small testicles, testicular atrophy and infertility. Lack of Face hair. Have male sex organs but Sterile. Normal Intelligence. 1/2000 Live birth
-
Turner's syndrome 45x monosomy
by a missing or incomplete X chromosome in females.

Inherited Mutation
Inherited Mutation
Linked to sex Chromesomes
SEX Chromosome
X
Recessive
Lesch-Nyhan Syndrome
X-linked recessive condition.
Due to mutation in HPRT gene on Xq26-27, leading to hyperuricaemia.
deficiency in the enzyme hypoxanthine-guanine phosphoribosyltransferase (HGPRT) def
build-up of uric acid in body fluids
Gout and kidney failure/renal insufficiency due to uric acid accumulation
extremely rare condition
Clinical features
Features: ferocious self-mutilation (lip biting, finger biting), aggression, severe mental retardation, dystonia, writhing movements, corticospinal tract signs, seizures.
Compulsive self-mutilation behaviour, especially biting of lips and fingers
severe intellectual disability
nearly exclusive to male
Compulsive self-mutilation behaviour, especially biting of lips and fingers
Dysarthria and choreoathetotic movements
Microcephaly
Orange uricosuric acid "sand" found in nappies during infancy
Spasticity
Seizures
prognosis is poor
with most affected individuals dying in early adulthood. Kidney failure secondary to infection or uric acid deposition is a common cause of death
management
Allopurinol can reduce uric acid levels
SSRIs for behavioural problems
Dietary control is not a treatment
Dominant
Fragile X
Y
Autosomal
Inheritance pattern Of mutation
Dominant
Tuberous Sclerosis Complex TSC
Genetics
Mutations in TSC1 chromosome 9q34 or TSC2 chromosome 16p133
Subtopic
Clinical Relevance
Known etiology of autism
Classic triad intellectual disability, seizures, hamartomas
Seizures more common with severe intellectual disability
Treatment Vigabatrin for infantile spasms
Kidney stones
Ash leaf spots
Hematoma is a benign mass in the brain lungs Abdomen
Huntington's Disease
Genetics
CAG trinucleotide repeat expansion in Huntingtin gene chromosome 4
Exhibits anticipation
Clinical Relevance
Cognitive impairment, depression, chorea
Juvenile onset 10% of cases early tics, rigidity, dystonia
Associated with caudate atrophy
DNA testing diagnostic and predictive
Frontotemporal Neurocognitive Disorder FTLD
Genetics
Up to 50% familial, mutations in several genes
Autosomal dominant MAPT chromosome 17, GRN chromosome 17
Clinical Relevance
Progressive behavioral changes, language decline
Impact on cognitive function and independence
EarlyOnset Familial Alzheimer's Disease eFAD
Genetics
Autosomal dominant missense mutations in PSEN1 chromosome 14, PSEN2 chromosome 1, APP chromosome 21
Aberrant cleavage of APP increases neurotoxic amyloid beta 42
Clinical Relevance
Primarily neurocognitive disorder dementia
Early onset leads to significant intellectual impairment
Williams Syndrome
Genetics
Microdeletion on chromosome 7q1123
supravalvular aortic stenosis, specific cardiovascular abnormalities.
Clinical Relevance
Psychiatric features anxiety, ADHD, poor judgment
Associated with anxiety disorder and phobias.
Associated with intellectual disability and speech problems
Cognitive: verbal skills often better than motor and visual spatial skills ("cocktail party speech").
hoarse voice,
Features: short stature, "elfin-like facies" (broad forehead),
Normal head circumference.
CADASIL
Genetics
Rare autosomal dominant mutation in Notch 3 gene chromosome 19q12
Clinical Relevance
Symptoms migraines, recurrent strokes, cognitive decline
Can cause intellectual disability if onset is early and severe
Kallmann Syndrome
Hypogonadotropic hypogonadism along with anosmia (impaired sense of smell), and occasionally learning difficulties.
M:F = 5:1.
Associated with Kiss1 gene mutations.
Recessive
Phenylketonuria PKU
Genetics Autosomal recessive
Clinical Relevance Untreated leads to severe intellectual disability treated with low phenylalanine diet
Wilson's Disease
Genetics Autosomal recessive defect in copper transporter on chromosome 13
Clinical Relevance Symptoms include dysarthria, tremor, psychiatric disease diagnostic tests include high urine copper
TaySachs Disease
Genetics Autosomal recessive disorder
Clinical Relevance Causes severe neurodegeneration and intellectual disability
Galactosemia
Genetics Autosomal recessive disorder
Clinical Relevance Untreated leads to intellectual disability
Maple Syrup Urine Disease
Genetics Autosomal recessive disorder
Clinical Relevance Untreated leads to intellectual disability
Homocystinuria
Genetics Autosomal recessive disorder
Clinical Relevance Untreated leads to intellectual disability
Biotinidase Deficiency
Genetics Autosomal recessive metabolic cause
Clinical Relevance Untreated leads to intellectual disability
Congenital Hypothyroidism
Genetics Autosomal recessive disorder
Clinical Relevance Untreated leads to significant intellectual disability
NiemannPick Disease Type C
Genetics Autosomal recessive disorder
Clinical Relevance Associated with intellectual disability and neurological degeneration
Friedreich's Ataxia
Genetics Autosomal recessive, inherited ataxia
Clinical Relevance Characterized by cerebellar degeneration and neuropsychological deficits
Personality Disorders
DSM5TR Classification
Overview of DSM5TR
Retains 10 specific personality disorders from DSMIV
Grouped into three clusters
Cluster A Odd or Eccentric
Paranoid Personality Disorder
Distrust and suspiciousness
Interpretation of others' motives as malevolent
Schizoid Personality Disorder
Detachment from social relationships
Restricted emotional expression
Schizotypal Personality Disorder
Acute discomfort in close relationships
Cognitive or perceptual distortions
Eccentricities of behaviour
Cluster B Dramatic, Emotional, or Erratic
Antisocial Personality Disorder
Disregard for the rights of others
Criminality and impulsivity
Failure to learn from experience
Borderline Personality Disorder
Instability in relationships and selfimage
Marked impulsivity
Histrionic Personality Disorder
Excessive emotionality
Attention seeking behaviour
Narcissistic Personality Disorder
Grandiosity and need for admiration
Lack of empathy
Cluster C Anxious or Fearful
Avoidant Personality Disorder
Social inhibition and feelings of inadequacy
Hypersensitivity to negative evaluation
Dependent Personality Disorder
Submissive and clinging behaviour
Excessive need for care
ObsessiveCompulsive Personality Disorder
Preoccupation with orderliness and perfectionism
Control issues
Alternative DSM5 Model for Personality Disorders
Overview of Alternative Model
Hybrid dimensionalcategorical approach
Criterion A Impairments in Personality Functioning
Evaluated on a continuum mild to extreme
Selffunctioning identity and selfdirection
Interpersonal functioning empathy and intimacy
Moderate impairment required for diagnosis
Criterion B Pathological Personality Traits
Organized into five domains
Negative Affectivity
Detachment
Antagonism
Disinhibition
Psychoticism
Personality DisorderTrait Specified PDTS
For cases not meeting criteria for specific disorders
Significant impairment and pathological traits present
Key Takeaways for MCQs
Important Pairings for Exam Preparation
Borderline PD with Splitting Highly tested pairing
Paranoid PD with Projection Another classic pairing
General Observations
Many personality disorders utilize immature defenses due to emotional dysregulation
Denial and regression can occur across disorders but are pervasive in personality disorders
Narcissistic and primitive defenses often overlap with immature defenses in context
Immature Defense Mechanisms and Personality Disorders
Borderline Personality Disorder BPD
Key Defenses
Splitting Major defense mechanism
Projective Identification Commonly used
Denial and Distortion Frequently observed
Dissociation Common under stress
Antisocial Personality Disorder ASPD
Key Defenses
Acting Out Direct expression of unconscious wishes
Projection Commonly used to deflect blame
Dissociation and Somatization Notable for coping with stress
Narcissistic Personality Disorder NPD
Key Defenses
Splitting Idealization and devaluation of self and others
Projection Shifting blame and feelings onto others
Paranoid Personality Disorder PPD
Key Defenses
Projection Most often associated with this disorder
Denial and Distortion Commonly utilized
Histrionic Personality Disorder HPD
Key Defenses
Regression Often seen in response to stress
Denial and Dissociation Used to manage emotional turmoil
Schizoid Personality Disorder SPD
Key Defenses
Projection Commonly employed
Schizoid Fantasy Retreating into fantasy to avoid conflict
Schizotypal Personality Disorder STPD
Key Defenses
Projection Frequently observed
Denial and Distortion Used to cope with reality
Avoidant Personality Disorder AVPD
Key Defenses
Projection Commonly utilized
Avoidance Key maladaptive strategy linked to phobias
Dependent Personality Disorder DPD
Key Defenses
Projective Identification Seeking validation through others
Somatization Physical symptoms as a way to express needs
Understanding Immature Defense Mechanisms in Personality Disorders
Definition of Immature Defense Mechanisms
Maladaptive behaviors leading to psychological distress
Regression Reverting to earlier behaviors under stress
Somatization Physical symptoms as a way to express unacknowledged needs
Acting Out Engaging in problematic activities to avoid feelings
Blocking Temporarily halting thoughts or feelings for protection
Key Immature Defense Mechanisms
Narcissistic or Primitive Defenses
Projection Attributing one's unacceptable feelings to others
Projective Identification Projecting feelings onto another who then expresses them
Splitting Viewing situations or people as all good or all bad
Denial Repressing unacceptable impulses or emotions
Distortion Reshaping reality to meet emotional needs
Dissociation Disconnecting from thoughts, feelings, or identity
Anxiety disorders
Panic Disorder
Diagnostic Criteria
Characterized by recurrent unexpected panic attacks
Persistent concern about additional attacks or maladaptive behavioral changes
Key Features 🏃♂️
Approximately 30% experience nocturnal panic attacks
Sufferers often focus on interoceptive cues and catastrophize mild physical sensations
Risk factors include smoking and childhood abuse
Treatment Approaches
Firstline Medications
SSRIs eg, fluoxetine, paroxetine, sertraline
SNRIs eg, venlafaxine XR are FDAapproved
Psychotherapy Techniques
Cognitive Behavioral Therapy CBT focusing on cognitive restructuring, exposure to interoceptive cues, relaxation training, and psychoeducation
Benzodiazepines
Used for acute relief but must be administered cautiously due to their properties anxiolytic, sedative, anticonvulsant, amnestic, muscle relaxant effects
Social Anxiety Disorder Social Phobia
Diagnostic Criteria
Marked fear or anxiety about one or more social situations where the individual may be scrutinized by others, fearing negative evaluation
Social situations are often avoided or endured with intense anxiety fear is disproportionate to the actual threat
Comorbidity Insights 📊
Commonly comorbid with avoidant personality disorder
Treatment Approaches
Medication Options
SSRIs eg, sertraline, paroxetine and SNRIs eg, venlafaxine are firstline, FDAapproved treatments
MAOIs are effective but carry safety concerns
Psychotherapy Techniques
Exposure therapy, cognitive therapy, and social skills training
Specific Phobia
Diagnostic Criteria
Marked fear or anxiety regarding a specific object or situation, provoking immediate fear/anxiety
The object/situation is actively avoided or endured with intense anxiety fear is out of proportion to actual danger, persisting for at least six months
Subtypes of Phobia 🐍
Animal
Natural environment
Bloodinjectioninjury
Situational
Other
Treatment Focus
Exposure therapy is the main treatment modality
Separation Anxiety Disorder
Diagnostic Criteria
Developmentally inappropriate and excessive fear or anxiety concerning separation from attachment figures
Adult Presentation Example
Can manifest in adults, such as a mother experiencing overwhelming anxiety about her schoolaged children
Overview of Anxiety Disorders
Definition and Characteristics
Defined by excessive fear and anxiety and related behavioral disturbances
Epidemiological Insights 🧠
High suicide risk associated with anxiety disorders
More prevalent in females compared to males
Chronic nature with episodes of waxing and waning
Neurotransmitter Involvement
Key neurotransmitters include norepinephrine, serotonin, GABA, and glutamate
Differential Diagnosis Ruleouts ⚠️
Medical Conditions
Cardiac issues eg, myocardial infarction, angina
Lung disorders eg, asthma
Endocrine disorders eg, pheochromocytoma, hyperthyroidism
Neoplasms eg, carcinoid syndrome
Neurological disorders eg, temporal lobe epilepsy, Huntington's disease
Electrolyte disturbances and B12 deficiency
Substance/MedicationInduced Conditions
Intoxication from stimulants, cocaine, hallucinogens, cannabis, nicotine, caffeine, and organophosphates
Withdrawal symptoms from alcohol, opiates, barbiturates, sedativehypnotics, SSRIs, and shortacting benzodiazepines like alprazolam
Generalized Anxiety Disorder GAD
Diagnostic Criteria
Excessive anxiety and worry occurring more days than not for at least six months about various events or activities
Difficulty controlling the worry, with at least three associated symptoms restlessness, fatigue, concentration difficulty, irritability, muscle tension, sleep disturbance
Treatment Options 💊
SSRIs eg, escitalopram, paroxetine and SNRIs eg, venlafaxine XR, duloxetine are FDAapproved
Buspirone is noted to be more effective for mental anxiety compared to somatic anxiety
Agoraphobia
Diagnostic Criteria
Marked fear or anxiety regarding at least two situations eg, public transport, open spaces, enclosed spaces, crowds, being outside home alone
Avoidance behavior or enduring situations with dread
Treatment Strategies 🏠
Similar to Panic Disorder, with an emphasis on exposure therapy to agoraphobic situations
Trauma and StressorRelated Disorders
PostTraumatic Stress Disorder PTSD
Diagnostic Criteria
Exposure to actual or threatened death, serious injury, or sexual violence, followed by symptoms from at least four clusters intrusion, avoidance, negative alterations in cognitions and mood, alterations in arousal and reactivity
Symptoms must persist for longer than one month
Specifiers 🧩
"With dissociative symptoms" depersonalization, derealization
"With delayed expression" full criteria not met until at least six months after trauma
Comorbidity Rates 📊
Very high, with 80% of individuals experiencing at least one other mental disorder commonly comorbid with MDD, SUDs, and anxiety disorders
Increased chronic risk of suicide and violence
Treatment Approaches
Traumafocused Cognitive Behavioral Therapy TFCBT is the firstline psychotherapy, especially for children and adolescents
Prazosin can be used for nightmares associated with PTSD
Psychological debriefing is NOT recommended as it may worsen symptoms benzodiazepines should be avoided due to increased PTSD risk
Acute Stress Disorder ASD
Diagnostic Criteria
Exposure to trauma with at least nine symptoms from five categories intrusion, negative mood, dissociative symptoms, avoidance, arousal
Duration is between three days and one month
Key Insight 🔑
Dissociative symptoms are a required criterion for ASD but a specifier for PTSD
Adjustment Disorder
Diagnostic Criteria
Development of emotional or behavioral symptoms in response to an identifiable stressor occurring within three months of its onset
Symptoms must be clinically significant marked distress or significant impairment in functioning
Key Insight 📅
Does not meet criteria for another mental disorder and is not an exacerbation of a preexisting mental disorder
Prognosis Insights
Good longterm prognosis for adult onset adolescent onset may progress to major psychiatric disorders
Trauma And stress
Overview of TraumaRelated Disorders
Definition
Resulting from exposure to a traumatic or stressful event
Acute Stress Disorder (ASD) and Its Comparison with Other Stress-Related Disorders
I Core Features of Acute Stress Disorder ASD
A Exposure to Trauma
1 Criteria require exposure to actual or threatened death, serious injury, or sexual violence
2 Can occur through direct experience, witnessing, learning about it, or repeated exposure to aversive details
B Symptom Categories
1 At least 9 symptoms from five categories
a Intrusion symptoms eg, distressing memories, dreams, flashbacks
b Negative mood
c Dissociative symptoms eg, depersonalization, derealization
d Avoidance
e Arousal symptoms eg, sleep disturbance, irritability
C Duration
1 Symptoms last from a minimum of 3 days to a maximum of 1 month posttrauma
2 This duration is the key differentiator from PTSD
D Impairment
1 Causes significant distress or impairment in functioning
E Exclusions
1 Not attributable to substance use, another medical condition, or brief psychotic disorder
II Comparison with PostTraumatic Stress Disorder PTSD
A Timeframe
1 ASD Symptoms last from 3 days to 1 month
2 PTSD Symptoms last longer than 1 month ASD often precedes PTSD
B Dissociative Symptoms
1 ASD Dissociative symptoms are a required criterion
2 PTSD Dissociative symptoms are a specifier, not a core requirement
C Clinical Picture in Children/Adolescents
1 Toddlers/Preschoolers May present as generalized anxiety or sleep disturbance
2 Schoolaged Children Avoidance/numbing less common sleep disturbance is common
3 Adolescents More common dissociative features, selfinjurious behavior, and substance abuse
D Differential with ADHD
1 Both can present with hyperarousal and distractibility
2 ADHD Symptoms are continuous
3 PTSD Hyperarousal is dependent on traumarelated cues
III Comparison with Adjustment Disorders
A Stressor Type
1 ASD Requires exposure to a lifethreatening traumatic event
2 Adjustment Disorder Develops in response to an identifiable, nonlifethreatening stressor
B Symptom Duration
1 ASD Symptoms resolve within 1 month
2 Adjustment Disorder Symptoms typically resolve within 6 months unless chronic
IV Neurobiological Correlates and Management
A Neurobiology of Trauma
1 Early and severe trauma can lead to elevated stress hormones
2 Impacts memory processing and brain functions, increasing psychiatric and physical illnesses
B Management of ASD
1 Psychological Debriefing Contraindicated may worsen symptoms
2 Firstline Psychosocial Treatment Cognitive Behavioral Therapy CBT including controlled exposure
3 Medication SSRIs, benzodiazepines use cautiously, secondgeneration antipsychotics, mood stabilizers, or betablockers for specific symptoms
Antidepressants in PostTraumatic Stress Disorder PTSD
Firstline Treatments
SSRIs sertraline, paroxetine, fluoxetine and SNRIs venlafaxine
TCAs desipramine and MAOIs phenelzine also effective
Sexual disorders
Sexual Dysfunctions
Definition and Characteristics
Clinically significant disturbance in sexual response or pleasure
Heterogeneous group of disorders affecting sexual functioning
Examples include erectile dysfunction, premature ejaculation, and sexual aversion
Contributing Factors
Relationship problems, substances, and medical conditions
Psychological factors such as anxiety or depression can exacerbate dysfunction
Certain medications and chronic illnesses may also play a role
Paraphilic Disorders
Definition and Features
Recurrent, intense sexually arousing fantasies or behaviors
Involves nonhuman objects, nonconsenting individuals, or suffering/humiliation
Almost always affect males, with a maletofemale ratio of 201 for masochism
Diagnostic Criteria
Duration of ≥6 months causing distress or impairment
Fantasies or urges are sufficient for diagnosis even without acted behaviors
Often comorbid with other paraphilic disorders
Pedophilic Disorder
Longterm, multimodal treatment approach
Goals include reducing sex drive and increasing inhibition to pedophilic behaviors
Treatment often mandated by the court system
Types of Paraphilic Disorders
Voyeuristic Disorder 👀
Definition and Characteristics
Voyeuristic disorder involves observing unsuspecting individuals engaged in intimate behaviors
This can include watching others undress, engage in sexual activity, or use the bathroom
The individual experiences sexual arousal from these observations, often leading to distress or impairment
Legal and Ethical Considerations
Voyeurism can lead to legal consequences, including charges of invasion of privacy
Many jurisdictions classify voyeuristic behavior as a criminal offense, especially when it involves minors
Ethical concerns arise regarding consent and the rights of the observed individuals
Exhibitionistic Disorder 🎭
Definition and Characteristics
Exhibitionistic disorder involves exposing one's genitals to unsuspecting individuals for sexual gratification
This behavior may occur in public places or through digital means, such as sending unsolicited explicit images
The thrill of being seen or the shock value often contributes to the arousal experienced by the individual
Psychological Factors
Individuals may engage in this behavior due to underlying issues such as low selfesteem or a desire for control
Exhibitionism may serve as a coping mechanism for feelings of inadequacy or social anxiety
Treatment often focuses on addressing these underlying psychological factors
Frotteuristic Disorder 🚆
Definition and Characteristics
Frotteuristic disorder involves rubbing against a nonconsenting person for sexual pleasure
This often occurs in crowded places, such as public transport, where the individual can blend in
The act of touching or grinding against someone else provides a sense of thrill and excitement
Social Implications
Frotteurism can lead to significant distress for victims, who may feel violated or unsafe
Legal consequences can include charges of sexual assault or harassment
Awareness campaigns are essential to educate the public about consent and personal boundaries
Sexual Masochism Disorder 🔗
Definition and Characteristics
Sexual masochism disorder involves deriving sexual pleasure from being humiliated, beaten, or otherwise made to suffer
This can include a wide range of activities, from light bondage to more extreme forms of pain
The individual may seek out partners who are willing to engage in these activities consensually
Consent and Safety
Consent is a critical component of sexual masochism, distinguishing between healthy practices and abusive behavior
Safe words and clear communication are essential to ensure the wellbeing of all parties involved
Education on BDSM practices emphasizes the importance of mutual consent and safety measures
Sexual Sadism Disorder 🔥
Definition and Characteristics
Sexual sadism disorder involves deriving sexual pleasure from inflicting pain or humiliation on others
This can manifest in various ways, including physical violence or psychological manipulation
The behavior becomes a disorder when it causes distress or impairment to the individual or their partner
Ethical Considerations
The line between consensual sadism and abuse can be blurred, raising ethical concerns
It is crucial to differentiate between consensual BDSM practices and nonconsensual acts of violence
Discussions around consent and power dynamics are essential in understanding sexual sadism
Fetishistic Disorder 👗
Definition and Characteristics
Fetishistic disorder involves sexual arousal from nonliving objects or specific body parts
Common fetishes include clothing items eg, lingerie, leather or body parts eg, feet
The fetish becomes a disorder when it significantly impairs functioning or causes distress
Cultural Perspectives
Fetishes can vary widely across cultures and may be influenced by societal norms and values
Understanding the cultural context of fetishes is essential for a comprehensive view of human sexuality
Some fetishes are more accepted in certain cultures, while others may be stigmatized
Transvestic Disorder 🌈
Definition and Characteristics
Transvestic disorder involves sexual arousal from crossdressing, typically associated with heterosexual males
The behavior may include wearing clothing typically associated with the opposite gender
This disorder is characterized by distress or impairment related to the crossdressing behavior
Gender Identity and Expression
Transvestism is distinct from transgender identity many individuals may crossdress without identifying as transgender
Understanding the nuances of gender identity is crucial in discussions about transvestic disorder
Support and acceptance are essential for individuals exploring their gender expression
Pedophilic Disorder 🚸
Definition and Characteristics
Pedophilic disorder involves sexual attraction to prepubescent children, typically 13 years old or younger
This disorder is considered one of the most serious due to the potential for exploitation and harm to minors
The individual may act on these urges or experience significant distress due to them
Legal and Social Implications
Pedophilia is illegal and heavily stigmatized, leading to severe legal consequences for offenders
Societal attitudes towards pedophilia are overwhelmingly negative, reflecting a strong protective instinct for children
Treatment options focus on managing urges and preventing harmful behaviors, often involving therapy and support groups
Paraphilic Disorders
Overview of Paraphilic Disorders
Definition of Paraphilic Disorders
Paraphilic disorders involve intense sexual urges, fantasies, or behaviors that deviate from societal norms
These disorders often lead to distress or impairment in social, occupational, or other important areas of functioning
Diagnostic criteria are outlined in the DSM5, emphasizing the need for the behavior to cause significant distress or impairment
Prevalence and Impact
Paraphilic disorders are relatively rare but can have significant implications for individuals and society
Estimates suggest that around 510% of the population may experience some form of paraphilia
The impact on relationships, mental health, and legal issues can be profound, especially in cases involving nonconsensual acts
Treatment and Management of Paraphilic Disorders
Therapeutic Approaches
Cognitive Behavioral Therapy CBT
CBT is commonly used to help individuals understand and manage their paraphilic urges
This approach focuses on identifying negative thought patterns and replacing them with healthier behaviors
Techniques such as exposure therapy may be employed to reduce arousal associated with specific stimuli
Medication
Pharmacological treatments may include antidepressants or antiandrogens to reduce sexual drive
Medications can help manage symptoms but are often used in conjunction with therapy for best results
Ongoing monitoring and adjustments may be necessary to achieve optimal outcomes
Support Systems
Peer Support Groups
Support groups provide a safe space for individuals to discuss their experiences and challenges
Sharing stories can foster a sense of community and reduce feelings of isolation
These groups often emphasize the importance of consent and healthy relationships
Family Involvement
Involving family members in treatment can provide additional support and understanding
Education for family members about the disorder can help reduce stigma and promote empathy
Open communication within families can facilitate healthier relationships and coping strategies
Conclusion
Importance of Awareness and Education
Increasing awareness about paraphilic disorders can reduce stigma and promote understanding
Education can empower individuals to seek help without fear of judgment
Encouraging open discussions about sexuality can foster a healthier societal perspective on diverse sexual behaviors
Future Directions
Ongoing research is essential to understand the complexities of paraphilic disorders better
Studies focusing on the biological, psychological, and social aspects can inform treatment approaches
Advocacy for mental health resources and support systems is crucial for individuals struggling with paraphilic disorders
Gender Dysphoria
Definition and Key Concepts
Marked incongruence between experienced gender and assigned gender
Chief diagnostic concept gender incongruence
May lead to significant distress or impairment in social, occupational, or other areas of functioning
Differential Diagnosis
Distinguishing from other disorders
Simple gender nonconformity in children
Body Dysmorphic Disorder and Schizophrenia delusional
Transvestic disorder focuses on sexual arousal rather than gender incongruence
Somatic symptoms disorder
Somatisation & Somatic Symptom Disorder (SSD
Historical Context of Somatisation
Definition of Somatisation
Experience of physical symptoms without sufficient physical cause
Symptoms attributed to physical illness with presumed psychological origin
Symptoms Focus
Patients preoccupied with diffuse, polysymptomatic complaints
Multiple organ systems affected eg, gastrointestinal, musculoskeletal 🏥
Course of Somatisation
Early onset typically before age 30
Chronic course, worsened by stress
Consciousness of Symptoms
Symptoms are not under voluntary control
Patients genuinely experience the symptoms
Associated Features
More common in women
Family history of alcohol use and antisocial personality disorder
Somatic Symptom Disorder SSD in DSM5
Key Concept of SSD
Shift from medically unexplained symptoms to maladaptive thoughts, feelings, and behaviors
Absorbed cases of "Hypochondriasis" and replaced "Somatization Disorder"
DSM5 Diagnostic Criteria
One or more distressing somatic symptoms disrupting daily life
Symptoms may or may not be linked to a diagnosed medical condition
Excessive thoughts, feelings, or behaviors related to symptoms
Disproportionate thoughts about seriousness of symptoms
Persistently high levels of health anxiety
Excessive time devoted to health concerns
Symptoms lasting more than 6 months
Psychological Features of SSD
Catastrophic interpretations of physical sensations
Appraisal of bodily symptoms as unduly threatening
Insight in SSD
Beliefs not held with delusional intensity
Patients can acknowledge the possibility of exaggeration
Specifiers for SSD
Can specify "with predominant pain"
Severity levels mild, moderate, severe
Hypochondriasis & Illness Anxiety Disorder IAD
Historical Context of Hypochondriasis
Key Concept of Hypochondriasis
Previously a distinct diagnosis in DSMIV
Now classified as either SSD or IAD in DSM5
Definition of Hypochondriasis
Preoccupation with fear of having a serious disease
Based on misinterpretation of bodily symptoms
Symptoms Focus
Focus on the idea of having or acquiring a serious illness
Specific illnesses often named eg, cancer 🦠
Insight in Hypochondriasis
Belief is not delusional patients can accept exaggeration
Reassurance Seeking Behavior
Persistent fears despite medical reassurance
Leads to "doctor shopping" or avoidance of medical contact
Illness Anxiety Disorder IAD in DSM5
Key Concept of IAD
Diagnosis for individuals with high health anxiety in absence of significant somatic symptoms
DSM5 Diagnostic Criteria
Preoccupation with having or acquiring a serious illness
Somatic symptoms absent or only mild
High anxiety about health easily alarmed
Excessive healthrelated behaviors eg, checking or maladaptive avoidance
Illness preoccupation lasting at least 6 months
Not better explained by another mental disorder
Functional Impact of IAD
Significant impairment in daily functioning
Negative effects on quality of life 🏆
Specifiers for IAD
Can specify as "careseeking type" or "careavoidant type"
How to Differentiate MCQfocused
Symptom Presence
Somatization Older
Many physical symptoms across multiple systems
Somatic Symptom Disorder SSD
One or more distressing somatic symptoms
Illness Anxiety Disorder IAD
Somatic symptoms absent or only mild
Primary Concern
Somatization Older
Preoccupation with the physical symptoms themselves
SSD
Focus on distressing symptoms and maladaptive thoughts/feelings
IAD
Preoccupation with the idea of having a serious illness 🧠
Delusional Intensity
SSD & IAD
Beliefs not held with delusional intensity acknowledgment of possible exaggeration
Duration of Symptoms
Somatization Older
Chronic, lasting for years
SSD & IAD
Persistent, typically for 6 months or more
Relation to Old Terms
SSD
Replaced "Somatization Disorder"
Subsumes about 75% of former "Hypochondriasis" cases
IAD
Subsumes about 25% of former "Hypochondriasis" cases
Sometimes referred to as "health anxiety"
Differentiating from Feigned Disorders
Somatic Symptom Disorder SSD / Illness Anxiety Disorder IAD
Consciousness of Symptoms
Symptoms genuinely experienced, not intentionally produced
Ekbomb
Fornication
A. Somatisation Disorder (Briquet's Syndrome)
Chronic disorder of multiple medically unexplained physical symptoms across various organ systems.
Most symptoms non-specific and atypical.
Associated with significant psychological distress and functional impairment.
Usually presents before age 40 (often
Symptoms are not intentionally produced or feigned.
B. Conversion Disorder (Functional Neurological Symptom Disorder)
Neurological symptoms (e.g., weakness, paralysis, pseudoseizures, blindness, involuntary movements, sensory disturbances) that cannot be explained medically, but are related to stress or conflict.
More common in women.
Classically associated with "La belle indifférence" (apparent lack of concern about symptoms), though not a diagnostic criterion.
Symptoms are unconscious and unintentional.
Differential diagnosis includes MS, GBS, CJD, dementia, brain tumors, myasthenia gravis, polymyositis.
D. Malingering
Conscious, intentional production of false or exaggerated physical/psychological symptoms.
Motivation is external gain (e.g., avoiding work, financial compensation, obtaining drugs, avoiding military service).
Resolution of symptoms when external gain is settled is a typical feature.
C. Factitious Disorder (Munchausen Syndrome)
Conscious, intentional production of false or exaggerated physical/psychological symptoms.
Motivation is to assume the "sick role" (primary gain), not external incentives.
Munchausen Syndrome by Proxy: Symptoms produced in another person under one's care (e.g., child).
F. Hypochondriasis (Illness Anxiety Disorder)
Preoccupation with having or acquiring a serious illness despite reassurance and lack of physical findings.
Disruptive impulse control Disorder
Oppositional Defiant Disorder ODD 😠
Criteria for Diagnosis
Pattern of angry/irritable mood, argumentative/defiant behavior, or vindictiveness lasting at least 6 months
Requires at least 4 symptoms eg, losing temper, easily annoyed, defying requests
Course and Prognosis
Approximately 25% will not have further diagnosis
3040% of boys with severe ODD may progress to Conduct Disorder
Conduct Disorder CD
Criteria for Diagnosis
Repetitive and persistent pattern of behavior violating the basic rights of others or societal norms
Examples include aggression towards people or animals, destruction of property, deceitfulness, and serious rule violations
Important Note
Antisocial Personality Disorder ASPD requires a childhood diagnosis of conduct disorder for its diagnosis
Intermittent Explosive Disorder IED 💥
Criteria for Diagnosis
Recurrent behavioral outbursts representing a failure to control aggressive impulses
Outbursts are grossly out of proportion to the provocation and are not premeditated
Causes significant distress or impairment in functioning
Comorbidities
High rates of depression, anxiety, substance use disorders, ADHD, ODD, CD, ASPD, and borderline personality disorder
Treatment Options
Psychotherapy Cognitive Behavioral Therapy CBT focusing on skill training and anger management
Medications SSRIs/SNRIs Fluoxetine is most supported as firstline treatment avoid benzodiazepines due to potential disinhibition
Kleptomania
Criteria for Diagnosis
Recurrent failure to resist impulses to steal objects not needed for personal use or monetary value
Increasing tension before the act and pleasure or relief during or after the act
Not committed out of anger or vengeance, and not explained by other disorders
Treatment Options
No standard randomized controlled trialsupported treatment
Options include antidepressants SSRIs
Differentiating Oppositional Defiant Disorder ODD and Conduct Disorder CD
Core distinction
Nature of behaviors
ODD involves defiance and oppositionality
CD involves more severe antisocial behaviors
Severity of symptoms
ODD symptoms tend to be less severe
CD symptoms involve violation of rights of others
The core distinction lies in the nature and severity of t
Key symptoms
ODD symptoms
Angry mood
Often loses temper
Is easily annoyed
Often angry and resentful
Argumentative behavior
Actively defies or refuses to comply
Argues with authority figures
Blames others for mistakes
Vindictiveness
Has been spiteful or vindictive
Often seeks revenge
CD symptoms
Aggression to people and animals
Bullies, threatens or intimidates others
Initiates physical fights
Uses a weapon that can cause serious harm
Destruction of property
Deliberately destroys others' property
Deceitfulness or theft
Breaks into houses, buildings, or cars
Lies to obtain goods or favors
Theft without confrontation
Serious violations of rules
Stays out at night despite parental prohibitions
Runs away from home
Frequently truant from school
Onset and development
ODD typically manifests in early childhood
Symptoms may precede those of CD
Can lead to CD if not addressed
CD often develops in later childhood or adolescence
More likely to be diagnosed after ODD
Can emerge from a more troubled background
Prognosis
ODD prognosis
Often improves with intervention
May evolve into CD if untreated
CD prognosis
Higher risk of developing antisocial personality disorder
More challenging to treat
Gender differences
ODD
More commonly diagnosed in boys than girls
CD
More pronounced gender differences in prevalence
Boys exhibit more overt behaviors, girls may exhibit relational aggression
Etiological factors
Genetic predisposition
Family history of mood disorders or antisocial behavior
Environmental influences
Exposure to violence
Family conflict or parenting styles
Neurobiological factors
Brain structure and function differences
Impulse control issues
Common pitfalls in diagnosis
Misinterpreting normative behavior as ODD
Distinguishing between typical defiance and clinical symptoms
Overlooking cooccurring disorders
Anxiety or mood disorders often comorbid with ODD and CD
Confusing developmental phases with disorders
Normal adolescent risktaking vs CD behaviors
Treatment approaches
ODD interventions
Parent training programs
Focus on improving parentchild communication
Establishing clear and consistent rules
Individual therapy
Cognitivebehavioral interventions
Anger management strategies
CD interventions
Multisystemic therapy
Engaging family, peers, and community in treatment
Skills training
Social skills development
Problemsolving skills
Importance of early intervention
Prevents escalation to more severe disorders
Encourages healthy behavioral development
Reduces longterm societal impacts
Multidisciplinary approach
Involvement of schools, parents, and healthcare providers
Coordination of treatment plans
Regular monitoring and adjustments to interventions
Cultural considerations
Understanding cultural background in behavior interpretation
Adjusting interventions based on cultural norms and values
Resources for further learning
American Psychiatric Association guidelines
Evidencebased research articles
Clinical case studies for practical insights
Disruptive, ImpulseControl, and Conduct Disorders
Overview of Disorders
Definition and Impact
Disorders characterized by problems in selfcontrol of emotions and behaviors
Can lead to significant social and personal issues
Dissociative Disorders
Dissociative Syndrome
E. Ganser's Syndrome
Rare dissociative disorder, considered hysterical.
Features: "approximate answers" (vorbeireden) to questions, clouding of consciousness with disorientation, psychogenic physical symptoms (e.g., analgesia, hyperaesthesia), and sometimes pseudohallucinations.
Patients are amnesic for their abnormal behavior.
G. Da Costa's Syndrome
Somatoform autonomic dysfunction disorder.
Characterized by cardiac symptoms (fatigue, breathlessness, palpitations, chest pain) for which no organic cause is found.
Historically called "soldiers heart".
Definition and Characteristics
Disruption in normal integration of consciousness, memory, identity, emotion, and behavior
Core etiology often linked to trauma eg, abuse, neglect
Symptoms typically begin in childhood, with a chronic course and high suicide attempt rates 70%
Assessment and Treatment
Rule out medical conditions and substance use
Treatment includes stabilization, psychotherapy, and grounding exercises
Avoid benzodiazepines, which may increase dissociation
Dissociative Identity Disorder DID
Criteria and Features
Disruption of identity with ≥2 distinct personality states
Gaps in recall inconsistent with ordinary forgetting
DID takes precedence over other dissociative disorders if criteria are met
Depersonalization/Derealization Disorder
Persistent experiences of depersonalization or derealization
Reality testing remains intact can be distressing and trigger hypochondriacal concerns
Dissociative Amnesia
Inability to recall important autobiographical information
Types localized, selective, generalized, and continuous amnesia
Differentiation from Neurocognitive Disorder NCD based on memory orientation
Sleep wake disorder
Insomnia Disorder 🌙
Criteria for Diagnosis
Predominant dissatisfaction with sleep quantity or quality
Difficulty initiating or maintaining sleep, or earlymorning awakening
Occurs at least 3 nights per week for a minimum of 3 months
Cooccurrence with Other Conditions
Often coexists with medical conditions, substance use disorders, or psychiatric disorders
Treatment should address both insomnia and cooccurring conditions for effective resolution
Treatment Options
Nonpharmacologic Sleep hygiene education, Cognitive Behavioral Therapy for Insomnia CBTI
Pharmacologic Use of hypnotics as needed
Narcolepsy
Criteria for Diagnosis
Recurrent periods of an irresistible need to sleep, lapsing into sleep, or napping during the day
Occurs at least 3 times per week for a minimum of 3 months
Presence of cataplexy or specific hypocretin deficiency findings
Pathophysiology
Associated with a deficiency in hypocretin orexin, a neuropeptide that regulates wakefulness
Treatment Options
Psychostimulants eg, dextroamphetamine, methylphenidate for daytime sleepiness
Hypnotics eg, sodium oxybate for nighttime sleep
Antidepressants to reduce REM sleep intrusions
Special prescribing precautions for sodium oxybate due to potential misuse
Circadian Rhythm SleepWake Disorders
Definition
Persistent or recurrent sleep disruption due to misalignment between the required sleepwake schedule and the individual's circadian rhythm
Examples
Shift work disorder, jet lag, and delayed sleep phase disorder
Parasomnias 😳
Characteristics
Abnormal behaviors, emotions, perceptions, or dreams occurring during sleep
Types of Parasomnias
NonREM Sleep Arousal Disorder Includes sleepwalking and sleep terrors
REM Sleep Behavior Disorder Involves repeated episodes of arousal during sleep associated with vocalization and complex motor behaviors
Often linked to synucleinopathies such as Parkinson's disease
Substance/MedicationInduced Sleep Disorder
Definition
Sleep disturbances caused by the effects of substances or medications
Examples
Alcohol, stimulants, and certain medications that interfere with normal sleep patterns
Sleep wake disorder
BreathingRelated Sleep Disorders
Types of Disorders
Includes Obstructive Sleep Apnea Hypopnea, Central Sleep Apnea, and SleepRelated Hypoventilation
Diagnosis
Diagnosed based on polysomnographic criteria, assessing airflow and respiratory patterns during sleep
Hypersomnolence Disorder 😴
Criteria for Diagnosis
Excessive daytime sleepiness despite a main sleep period of at least 7 hours
Prolonged nighttime sleep or difficulty being fully awake after abrupt awakening
Occurs at least 3 times per week for a minimum of 3 months
Definition and Impact
Persistent disturbances in sleepwake patterns causing distress or functional impairment
Affects quality of life and daily functioning
Culture-Bound Syndromes
D. Koro
Mainly Asia.
Intense anxiety centered on the belief that the genitalia are retracting and their disappearance will cause death.
Not delusional (associated with local tradition that ghosts have no genitals).
G. Dhat Syndrome
South Asia.
Psychosexual disorder with anxiety about loss of semen.
I. Windigo
Native American Indians.
Delusional fear of being turned into a cannibal through possession by a supernatural monster.
H. Couvade Syndrome
Sympathetic pregnancy affecting husbands (rarely other family members) during their wives' pregnancies (most frequent between 3-9 months).
F. Piblokto (Arctic Hysteria)
Female Eskimos of northern Greenland.
Anxiety, depression, confusion, depersonalization, derealization, ending in stuporous sleep and amnesia.
E. Brain Fag Syndrome
Mainly African students.
Concentration difficulties, vague somatic complaints, and depressed mood.
C. Latah
Asia and North Africa.
Response to intense stress characterized by altered consciousness, hypersuggestibility, and mimicry (echolalia, echopraxia).
B. Ataque de Nervios
Hispanic American groups.
Grief reaction with fluctuating conscious level (amnesia), crying, shouting, trembling, difficulty moving limbs.
Hyperventilation may precipitate symptoms.
A. Amok
Sudden onset of uncharacteristic psychomotor excitement with marked violence (homicidal/suicidal) and paranoid symptoms, followed by amnesia.
Described in Africa, Asia, New Guinea as a response to humiliation.
def
Patterns of symptoms or abnormal behavior recognized as illnesses in specific cultures (in ICD-10, coded under existing disorders like dissociative or somatoform).