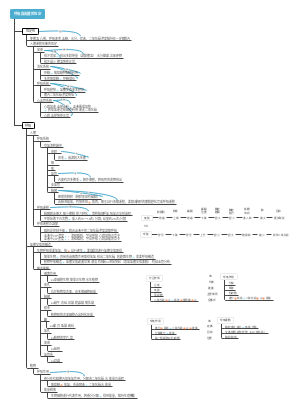
MindMap Gallery Physiology-Respiratory System
- 240
- 1
Physiology-Respiratory System
This is a mind map about physiology-respiratory system, including pulmonary ventilation, lung ventilation and tissue ventilation, gas transportation in the blood, regulation of respiratory movements, etc.
Edited at 2024-01-27 13:29:51- 30 Creative Ideas for Valentine's Day
This Valentine's Day map illustrates love through 30 romantic possibilities, from the vintage charm of "handwritten love letters" to the urban landscape of "rooftop sunsets," from the tactile experience of a "pottery workshop" to the leisurely moments of "wine tasting at a vineyard"—offering a unique sense of occasion for every couple. Whether it's cozy, experiential, or luxurious, love always finds the most fitting expression. May you all find the perfect atmosphere for your love story.
- Milano Cortina 2026 Ice Hockey Schedule
The ice hockey schedule for the Milano Cortina 2026 Winter Olympics, featuring preliminary rounds, quarterfinals, and medal matches for both men's and women's tournaments from February 5–22. All game times are listed in Eastern Standard Time (EST).
- 2026 Personal Annual Planning Handbook
This 2026 planner effectively combines goal setting with practical tools, including monthly plans, weekly plans, and monthly reviews. Integrated lifestyle and leisure sections ensure work-life balance, while the quarterly layout provides a clear structure for tracking progress. The planner's simple and clear design helps you clarify your goals, cultivate habits, and cherish every important moment – turning your plans into reality step by step, with new achievements every week.
Physiology-Respiratory System
- 30 Creative Ideas for Valentine's Day
This Valentine's Day map illustrates love through 30 romantic possibilities, from the vintage charm of "handwritten love letters" to the urban landscape of "rooftop sunsets," from the tactile experience of a "pottery workshop" to the leisurely moments of "wine tasting at a vineyard"—offering a unique sense of occasion for every couple. Whether it's cozy, experiential, or luxurious, love always finds the most fitting expression. May you all find the perfect atmosphere for your love story.
- Milano Cortina 2026 Ice Hockey Schedule
The ice hockey schedule for the Milano Cortina 2026 Winter Olympics, featuring preliminary rounds, quarterfinals, and medal matches for both men's and women's tournaments from February 5–22. All game times are listed in Eastern Standard Time (EST).
- 2026 Personal Annual Planning Handbook
This 2026 planner effectively combines goal setting with practical tools, including monthly plans, weekly plans, and monthly reviews. Integrated lifestyle and leisure sections ensure work-life balance, while the quarterly layout provides a clear structure for tracking progress. The planner's simple and clear design helps you clarify your goals, cultivate habits, and cherish every important moment – turning your plans into reality step by step, with new achievements every week.
- Recommended to you
- Outline
breathe
Overview
external breathing
pulmonary ventilation
Gas exchange between the alveoli and the external environment
lung ventilation
gas exchange between alveoli and pulmonary capillaries
gas transport
Transport of oxygen and carbon dioxide in the blood
internal breathing
tissue ventilation
gas exchange between tissue cells and tissue capillaries
Oxidative metabolism in tissue cells
pulmonary ventilation
organ
respiratory tract
Nose, pharynx, larynx, trachea, bronchi
Alveoli, pleural space, diaphragm, thorax
Principles of pulmonary ventilation
The power of pulmonary ventilation
direct power
The pressure difference between alveolar air and the outside atmosphere
The atmospheric pressure is constant, and the intrapulmonary pressure changes - the expansion and contraction of the lungs changes the intrapulmonary pressure - the rhythmic expansion and contraction of the thorax changes the lungs - caused by the contraction and relaxation of the respiratory muscles
driving force
Rhythmic respiratory movements caused by contraction and relaxation of respiratory muscles
respiratory movements
definition
The rhythmic expansion and contraction of the thorax caused by the contraction and relaxation of respiratory muscles is called respiratory movement
process
Inspiratory movement
active process
Contraction of inspiratory muscles (diaphragm and external intercostal muscles)
The chest cavity enlarges and the lung volume increases
Intrapulmonary pressure decreases below atmospheric pressure
outside air flows into the lungs
exhalation exercise
passive process
inspiratory muscle relaxation
The retraction force of the lungs recollects and pulls the thorax
Decreased chest and lung volumes
Intrapulmonary pressure is higher than atmospheric pressure
form
Muscle contraction
abdominal breathing
Mainly diaphragm relaxation and contraction activities
Pleural effusion, pleurisy, abdominal breathing in infants and young children
chest breathing
Mainly relax and contract activities of external intercostal muscles
Late pregnancy, huge abdominal mass, ascites, flatulence, peritonitis, chest breathing
Breathe calmly and breathe hard
calm breathing
12-18 times/minute
Breathe hard
Breathe in hard
Diaphragm and external intercostal muscles contract, sternocleidomastoid and scalene muscles contract
Exhale forcefully
Inspiratory muscles relax and expiratory muscles (abdominal muscles and internal intercostal muscles) contract
intrapulmonary pressure
pressure of gas in alveoli
Inhale
Increased lung volume
Reduced intrapulmonary pressure
below atmospheric pressure
gas in lungs
exhale
Reduced lung volume
increased intrapulmonary pressure
above atmospheric pressure
Gas leaving the lungs
intrapleural pressure
pleural cavity
A closed, potential, gas-free and small amount of serous fluid space between the visceral pleura on the lung surface and the parietal pleura on the inner wall of the thorax
intrapleural pressure
negative pressure
The intrapleural pressure at the end of quiet breathing is 3-5mmHg lower than the atmospheric pressure, and at the end of inspiration is 5-10mmHg lower than the atmospheric pressure.
Intrapleural pressure = atmospheric pressure (-pulmonary retraction pressure)
If you are breathing calmly and the atmospheric pressure is 0
Intrapleural pressure = - Pulmonary retraction pressure
significance
Expand lungs
dilation of vena cava and thoracic duct
Conducive to the return of venous blood and lymph fluid
resistance to pulmonary ventilation
Elastic resistance (70%) and compliance
Compliance
elastic resistance
The force of an elastic body against deformation caused by external forces is called elastic resistance
Also called lung retraction, it is the resistance to inhalation and the power to exhale.
Compliance
The ease with which elastic tissue deforms under the action of external forces
Large compliance, small elastic resistance Small compliance, large elastic resistance
Lung elastic resistance and lung compliance (0.2L/cmH2O)
lung compliance
static compliance
Compliance measured without airflow in the respiratory tract
Lung compliance C (L) = change in lung volume/change in transpulmonary pressure
When breathing calmly, the elastic resistance of the lungs is smaller and breathing is less laborious.
Effect of total lung volume on lung compliance
Specific compliance = lung compliance/total lung capacity
Used to compare the lung elastic resistance of individuals with different total lung volumes
Calm breathing begins with functional residual capacity
Specific compliance = lung compliance during quiet breathing/functional residual capacity
Sources of pulmonary elastic resistance
Alveolar surface tension 2/3
The force originating from the liquid-air interface on the inner surface of the alveoli that reduces the surface area of the liquid
Alveolar surface tension contributes to lung retraction
The retraction force of small alveoli is large, and the retraction force of large alveoli is small.
pulmonary surfactant
A mixture of lipids (90% dipalmitoyl lecithin DPPC) and proteins (10% surfactant binding protein SP) synthesized and secreted by alveolar type II epithelial cells
effect
Reduce alveolar surface tension and reduce alveolar recoil
Reduce inspiratory resistance and reduce inspiratory work
Maintain the stability of alveoli of different sizes
When exhaling, the alveoli shrink, the density of pulmonary surfactant increases, the surface tension reduction effect is enhanced, the lung retraction force is reduced, and it is easier to expand, thus preventing alveolar collapse, and vice versa.
Prevent pulmonary edema
Reduce alveolar surface tension, weaken the suction effect of surface tension on pulmonary capillaries (plasma) and lung interstitial fluid (interstitial fluid), prevent liquid from penetrating into the alveoli, and prevent the occurrence of pulmonary edema
Special groups
infants
Pulmonary surfactant begins to be synthesized and secreted at six or seven months
premature baby
Lack of pulmonary surfactant
Extremely narrowed alveoli and atelectasis
Attracts plasma from pulmonary capillaries into the alveoli, forming a transparent membrane on the inner wall of the alveoli, hindering gas exchange
Neonatal Respiratory Distress Syndrome (NRDS)
Pulmonary congestion, pulmonary tissue fibrosis, and decreased pulmonary surfactant
Decreased lung compliance
Increased elastic resistance
Difficulty breathing in
Emphysema
The elastic components of the lungs are greatly destroyed, the retraction force of the lungs is reduced, the compliance is increased, the elastic resistance is reduced, and it is difficult to exhale.
elastic component of the lungs
Lung's own elastic fibers and collagen fibers
The greater the lung expansion, the stronger the pulling effect, and the greater the lung retraction force and elastic resistance.
Thoracic elastic resistance and thoracic compliance (0.2L/cmH2O)
Quiet end-inspiration
Lung capacity is 67% of total lung capacity
There is no deformation of the thorax and no elastic resistance.
Breathe out calmly or deeply
Lung capacity is less than 67% of total lung capacity
The thorax is pulled inwards and narrows
elastic resistance outward
The force of inhalation, the resistance of exhalation
Take a deep breath
Lung capacity is 67% greater than total lung capacity
The thorax is pulled outward to expand
elastic resistance inward
resistance to inhalation, motivation to exhale
Total elastic resistance and total compliance of the lungs and thorax (0.1L/cmH2O)
Inelastic resistance (30%)
Airway resistance (80-90%)
The resistance caused by the friction between gas molecules and between gas molecules and the airway wall when gas flows through the respiratory tract.
Airway resistance = difference between atmospheric pressure and intrapulmonary pressure/gas flow per unit time
Influencing factors
Airway caliber (main)
Influencing factors
transmural pressure
pressure difference between inside and outside respiratory tract
The airway pressure is high, the transmural pressure is high, the airway caliber is passively expanded, and the airway resistance is small
Traction of the lung parenchyma on the airway wall
The traction effect of small airway elastic fibers and collagen fibers on the airway wall
Regulation of the autonomic nervous system
Sympathetic nerve
Airway smooth muscles relax, the diameter becomes larger, and airway resistance decreases
parasympathetic nerve
Airway smooth muscle contracts, the diameter becomes smaller, and airway resistance increases
The influence of chemical factors
Catecholamines
airway smooth muscle relaxation
prostaglandins
Histamine and leukotrienes
bronchoconstriction
endothelin
airway smooth muscle contraction
Why Asthma People Have More Difficulty Exhaling Than Inhaling
Inhale
Increased negative pressure in the pleural cavity and increased transmural pressure
The elastic component of lung expansion enhances the traction effect on small airways
Increased sympathetic nervous activity
Airway diameter increases and airway resistance decreases
Air velocity
Airflow pattern
inertial resistance
The force that prevents lung ventilation due to the inertia of the airflow and tissue when the airflow is started, changed speed, and reversed.
viscous drag
Friction from the relative displacement of tissues during breathing
Evaluation of pulmonary ventilation function
Overview
restrictive hypoventilation
Ventilator paralysis, expansile changes in the lungs and thorax, pneumothorax
Limited lung expansion
obstructive hypoventilation
Bronchial smooth muscle spasm, foreign bodies in the airway, excessive secretion of tracheal and bronchial mucosal glands, and compression by tumors outside the airway causing caliber reduction or airway obstruction
lung volume and total lung capacity
lung volume
The amount of gas the lungs can hold under different conditions
Tidal volume (TV)
definition
The amount of air inhaled or exhaled with each breath
normal value
400~600ml
Inspiratory supplementary volume (IRV)
definition
At the end of your quiet inhalation, try your best to inhale as much air as you can
normal value
1500-2000ml
significance
Reserve volume for reaction inspiration
expiratory supplementary volume (ERV)
definition
Calm down at the end of expiration, and then exhale as hard as you can.
normal value
900~1200ml
significance
Reflects the reserve volume of exhalation
Remaining air volume (RV)
definition
The amount of air that remains in the lungs at the end of maximum expiration and cannot be exhaled anymore
normal value
1000~1500ml
significance
Prevent alveolar collapse under low lung volume conditions
Lung capacity
The combined gas volume of two or more items in lung volume
Deep inspiratory volume (IC)
definition
Maximum amount of air that can be inhaled during quiet end-expiration
The sum of tidal volume and supplementary inspiratory volume
significance
One of the indicators of maximum ventilation potential
It can be reduced when lesions occur in the thorax, pleura, lung tissue and respiratory muscles.
Functional residual capacity (FRC)
definition
The amount of air remaining in the lungs at the end of quiet expiration
The sum of residual volume and expiratory volume
normal value
2500ml
significance
physiological significance
Buffers the changes in the alveolar oxygen partial pressure and carbon dioxide partial pressure during breathing. The alveolar air and arterial blood oxygen partial pressure will not fluctuate greatly with breathing, which is beneficial to lung ventilation.
Pathological significance
Patients with emphysema have increased functional residual capacity and decreased lung parenchymal lesions.
Vital capacity, forced vital capacity and forced expiratory volume
Vital capacity (VC)
definition
The maximum amount of air that can be exhaled from the lungs after inhaling as hard as possible
Tidal volume, supplementary inspiratory volume, sum of supplementary expiratory volumes
normal value
Men: 3500ml, women: 2500ml
significance
Reflects the maximum capacity of the lungs for primary ventilation
Forced vital capacity (FVC)
definition
After one maximum inhalation, try to exhale the maximum amount of air as quickly as possible
Forced expiratory volume (FEV)
definition
Try to exhale as quickly as possible after one maximum inhalation. The amount of gas that can be exhaled within a certain period of time.
normal value
FEV1/FVC 83%, FEV2/FVC 96%, FEV3/FVC 99%
significance
chronic obstructive pulmonary disease (asthma)
FEV1/FVC becomes smaller and the remaining air volume increases
Chronic restrictive lung disease (pulmonary fibrosis)
Both FEV1 and FVC decrease, FEV1/FVC can be basically normal, and the remaining air volume decreases.
total lung capacity (TLC)
definition
The maximum amount of gas the lungs can hold
The sum of vital capacity and residual capacity
normal value
Adult men 5000ml, women 3500ml
significance
Reduced total lung capacity during restrictive hypoventilation
Determination of functional remaining air volume
Helium dilution method
Pulmonary ventilation and alveolar ventilation
pulmonary ventilation
definition
The total amount of air inhaled or exhaled per minute
The product of tidal volume (500ml) and respiratory rate (12-18 times/min)
normal value
6~9L/min
alveolar ventilation
physiological dead space
anatomical dead space
Part of the inhaled gas remains in the respiratory tract between the nose or mouth and the terminal bronchioles, and does not participate in gas exchange between the alveoli and blood.
alveolar dead space
The gas entering the alveoli cannot all be exchanged with the blood due to the uneven distribution of blood flow in the lungs. The volume of the alveoli that cannot be exchanged is called the alveolar dead space.
definition
The amount of fresh air inhaled into the alveoli per minute
(tidal volume – dead space volume) × respiratory rate
normal value
4.2~6.3L/min
Maximum expiratory flow-volume curve
definition
After the subject inhales with all his strength, he tries to exhale as quickly as possible to the remaining volume. The exhaled air volume and flow rate are simultaneously recorded and drawn into a maximum expiratory flow rate-volume (MEFV) curve.
airway reactivity measurement
Also called bronchial provocation test (BPT)
A test that measures the degree of contraction of the bronchial tubes in response to inhalation of an irritating substance.
Inhale a certain amount of stimulant (histamine or acetylcholine) by atomization, and compare the pulmonary ventilation function indicators before and after inhalation, such as FEV1
PC20
The stimulant concentration that causes a 20% decrease in FEV1
Determine the diagnosis and prognosis of asthma (overreaction due to airway inflammation)
Breathing work
The work done by respiratory muscles to overcome ventilation resistance to achieve pulmonary ventilation during respiratory movements
Lung ventilation and tissue ventilation
Basic principles of gas exchange
diffusion of gas
Overview
There are partial pressure differences in different areas, and there is a net transfer of gas molecules from areas with high pressure to areas with low pressure.
partial pressure difference of gas
The partial pressure of a gas is equal to the total pressure of the mixed gas multiplied by the volume percentage of the gas in the mixed gas
The gas partial pressure difference is the difference in the partial pressure of a certain gas between two areas. It is the driving force for gas diffusion and a key factor in determining the direction of gas diffusion.
Molecular weight and solubility of gases
The diffusion coefficient of carbon dioxide is about 20 times that of oxygen
Carbon dioxide is 24 times more soluble in plasma than oxygen
temperature
Diffusion area and distance
Partial pressure of respiratory gases and gases in different parts of the human body
Composition and partial pressure of respiratory air and alveolar air
Breathing air
Inspired air
Air
The plateau has low atmospheric pressure and low gas partial pressure
Respiratory water vapor
exhale
Inspiratory air and part of alveolar air in dead space
Partial pressure of blood gases and tissue gases
lung ventilation
lung ventilation process
oxygen
Venous blood (PO2 40mmHg) → Alveoli (PO2 102mmHg) → Gas exchange (alveoli to blood) → Arterial blood
carbon dioxide
Venous blood (PCO2 46mmHg) → Alveoli (PCO2 40mmHg) → Gas exchange (blood to alveoli)
Factors affecting pulmonary ventilation
thickness of respiratory membrane
Respiratory membrane (air-blood barrier)
Liquid layer containing pulmonary surfactant → Alveolar epithelial cell layer → Epithelial basement membrane layer → Gap between epithelial basement membrane and capillary basement membrane → Capillary basement membrane layer → Capillary endothelial cell layer
The thicker the respiratory membrane, the longer it takes for diffusion and the smaller the amount of gas exchanged per unit time.
significance
pulmonary fibrosis, pulmonary edema
The respiratory membrane thickens and the diffusion distance increases
Gas diffusion rate decreases
Reduced diffusion
respiratory membrane area
The larger the diffusion area, the greater the diffusion rate
significance
Atelectasis, lung consolidation, emphysema, lobectomy, pulmonary capillary closure and obstruction
Respiratory membrane area decreases
Decreased diffusion rate
ventilation/blood flow ratio
definition
The ratio of alveolar ventilation per minute to pulmonary blood flow per minute
normal value
4.2/5=0.84
significance
Ratio increases
Hyperventilation or relative lack of blood flow
Part of the alveolar gas fails to fully exchange with blood gas
Alveolar dead space enlargement
Ratio decreases
Insufficient ventilation or relatively high blood flow
Part of the blood flows through the poorly ventilated alveoli, and the gases in the mixed venous blood cannot be fully renewed.
Functional arteriovenous short circuit
Gas exchange efficiency will be reduced, leading to hypoxia or carbon dioxide retention in the body.
V(A)/Q abnormality mainly manifests as hypoxia
The difference in oxygen partial pressure between arterial and venous blood is much greater than the difference in carbon dioxide partial pressure
The decrease in oxygen partial pressure is greater than the increase in carbon dioxide partial pressure
The diffusion coefficient of carbon dioxide is 20 times that of oxygen
Carbon dioxide diffuses quickly and is not easily retained
Decreased arterial blood oxygen partial pressure and increased carbon dioxide partial pressure can stimulate breathing, increase alveolar ventilation, and help carbon dioxide discharge
lung diffusion capacity
definition
The number of milliliters of gas that diffuses through the respiratory membrane per minute under the action of unit partial pressure difference is called lung diffusion capacity.
significance
A measure of the ability of respiratory gases to pass through the respiratory membrane
tissue ventilation
definition
Gas exchange between blood and tissue cells in systemic capillaries
Transport of gases in the blood
Overview
Both oxygen and carbon dioxide are transported in two forms: physically dissolved and chemically combined (primarily)
Only 1.5% of O₂ in blood is transported in physically dissolved form, and the remaining 98.5% is transported in chemically bound form.
oxygen transport
Molecular structure of Hb
1 globin and 4 heme. The heme center is a ferrous iron → the ferrous iron is combined with O₂ → Hb is called oxyhemoglobin HbO₂ (Hb without O₂ is called deoxygenated hemoglobin Hb)
HbO₂ bright red, Hb purple-blue
The combination or dissociation of Hb and O₂ will affect the formation or breakage of salt bonds, causing Hb to undergo an allosteric effect, causing its affinity with O₂ to change accordingly.
Characteristics of Hb binding to oxygen
Binding reaction is rapid and reversible
Binding and dissociation do not require enzyme catalysis and are affected by PO₂
Blood flows through the lungs with high PO₂, and Hb combines with oxygen
Blood flows through tissues with low PO₂, and HbO₂ is rapidly dissociated
The binding reaction is oxygenation rather than oxidation
Oxygenate rather than oxidize, deoxygenate rather than reduce
The amount of Hb combined with O₂
One molecule of Hb can bind 4 molecules of O₂, and 1gHb can bind the maximum amount of O₂ 1.39ml. Normally, red blood cells contain a small amount of high-iron Hb that cannot bind O₂, and the actual amount of O₂ bound is 1.34ml.
Hb oxygen capacity
definition
The maximum amount of O₂ that Hb can bind to in 100ml of blood
normal value
1.34×15 (100ml blood Hb concentration 15g/ml) = 20.1ml/100ml
Hboxygen content
definition
The amount of O₂ actually bound to Hb in 100ml of blood
normal value
arterial blood
19.4ml/100ml
venous blood
14.4ml/100ml
Hb oxygen saturation
definition
The percentage of Hb oxygen content and Hb oxygen capacity
Cyanosis
definition
The Hb content in the blood reaches more than 5g/100ml, and the skin and mucous membranes turn dark purple, which is cyanosis.
visible in
body hypoxia
Cyanosis without hypoxia
high altitude polycythemia
Hypoxia and acyanosis
Severe anemia or CO poisoning
The oxygen dissociation curve is S-shaped
Hb is a tight type (T type), HbO₂ is a loose type (R type)
Hb binds to O₂→T type changes to R type→The affinity for O₂ gradually increases
Hb dissociates from O₂ → R-type transforms into T-type → affinity to O₂ gradually decreases
oxygen dissociation curve
definition
The curve showing the relationship between blood PO₂ and Hb oxygen saturation, also called oxyhemoglobin dissociation curve
The upper part of the oxygen dissociation curve
Blood PO₂Hb oxygen saturation between 60~100mmHg
Features
The curve is flatter
Within this range, PO₂ has little effect on Hb oxygen saturation or blood oxygen content.
V/Q mismatch, pulmonary ventilation increases, oxygen uptake does not increase
PO₂ is 100mmHg, blood oxygen saturation is 97.4%, blood oxygen content is 19.4/100ml blood
PO₂ is 150mmHg, blood oxygen saturation is 100%, blood oxygen content is 20.0/100ml blood
As long as the arterial blood PO₂ is not less than 60mmHg, the Hb oxygen saturation can still be maintained above 90%, and the blood can carry a sufficient amount of O₂ without causing obvious hypoxemia.
The middle section of the oxygen dissociation curve
Blood oxygen saturation between PO₂40~60mmHg
Features
The curve is steeper
O₂ supply of blood to tissues under resting conditions
The lower part of the oxygen dissociation curve
Blood PO₂ blood oxygen saturation between 15~40mmHg
Features
steepest
Reflects the reserve capacity of blood to supply O₂
Factors Affecting Oxygen Dissociation Curve
P50
PO₂ when blood oxygen saturation reaches 50%, normal is about 26.5mmHg
Increase → the curve shifts to the right (PCO₂ increases, pH decreases, 2,3-DPG concentration increases, temperature increases) → Hb affinity with oxygen decreases
Higher PO₂ is required to achieve Hb oxygen saturation of 50%
Decrease → the curve shifts to the left (PCO₂ decreases, pH increases, 2,3-DPG concentration decreases, temperature decreases) → Hb affinity with oxygen increases
Lower PO₂ is required to achieve Hb oxygen saturation of 50%
Effect of blood pH and PCO₂
pH
bohr effect
Effects of blood acidity and PCO₂ on the affinity of Hb and O₂
The increase in acidity promotes the transformation of Hb to T-type and reduces the affinity for O₂
The acidity decreases, which promotes the transformation of Hb to the R form and increases the affinity for O₂
PCO₂
An increase in carbon dioxide partial pressure → corresponds to a decrease in pH
significance
Blood flows through the lungs → CO₂ transfers from the blood to the lungs → Blood PCO₂ decreases and pH increases → Hb’s affinity for O₂ increases → the curve shifts to the left → oxygen uptake is promoted and blood oxygen content increases
Blood flows through the tissue → CO₂ diffuses from the tissue to the blood → Blood PCO₂ increases and pH decreases → Hb’s affinity for O₂ increases → the curve shifts to the right → promotes HbO₂ dissociation and provides O₂ to the tissue
Effect of temperature
Increase in temperature → increase in hydrogen ion activity → decrease in affinity for oxygen
2,3-bisphosphoglycerate in red blood cells
Chronic hypoxia, anemia, high mountain hypoxia → Enhanced glycolysis → Increased red blood cell 2,3-DPG → Shift the oxygen dissociation curve to the right → Promote the release of oxygen from HbO₂
The anticoagulant citrate-glucose solution stores blood for more than 3 weeks → glycolysis stops → 2,3DPG concentration decreases → affinity increases and is not easy to dissociate, affecting tissue oxygen supply
Effects of carbon monoxide
The affinity between CO and Hb is about 250 times that of O₂
CO combines with one heme of the Hb molecule, increasing the affinity of the other three hemes for O₂ → the oxygen dissociation curve shifts to the left, hindering the dissociation of Hb and O₂
The combination of Hb and CO shows cherry color, CO poisoning, and lack of oxygen without cyanosis.
Hb combines with CO, PO₂ may be normal, it will not stimulate respiratory movement and increase pulmonary ventilation, but may inhibit the respiratory center, reduce pulmonary ventilation, and aggravate hypoxia
For CO poisoning, add 5% CO₂ to stimulate respiratory movements and treat it with hyperbaric oxygen therapy
other factors
transport of carbon dioxide
Transport forms of carbon dioxide
5% physical solution, 88% bicarbonate, 7% carbamoyl hemoglobin
Bicarbonates
In tissues, plasma or red blood cells, under the catalysis of carbonic anhydrase, carbon dioxide combines with water to form carbonic acid, and carbonic acid dissociates into bicarbonate and hydrogen ions.
Carbonic anhydrase inhibitor-acetazolamide
within the organization
CO₂ diffused into the blood through tissue ventilation is dissolved in the plasma
small portion
Lack of carbonic anhydrase in plasma
Catalyzed by carbonic anhydrase, carbon dioxide combines with water to form carbonic acid, which dissociates into bicarbonate and hydrogen ions.
Bicarbonate combines with sodium ions, NaHCO3
Hydrogen ions are buffered
most
Red blood cells contain high concentrations of carbonic anhydrase
Diffusion into red blood cells
Carry out reaction, the speed can be increased 5000 times
In the lungs, hydrogen ions and bicarbonate form carbonic acid, and carbonic acid dissociates into water and carbon dioxide
Carbamoyl hemoglobin HbO₂
oxygenation regulation
The production of HbO₂ in the lungs increases, which promotes the dissociation of HbCO₂ and releases CO₂, accounting for 17.5% of the CO₂ released in the lungs.
Rapid, efficient, reversible, no need for enzyme catalysis
carbon dioxide dissociation curve
Curve showing the relationship between CO₂ content in blood and PCO₂
Blood flows through the lungs, and the blood can release 4mlCO₂
Factors affecting carbon dioxide transport
major factor
Does Hb combine with O₂?
The combination of Hb and O₂ promotes the release of CO₂, and the Hb that releases O₂ easily combines with CO₂
Holden effect
Regulation of respiratory movements
Respiratory center and formation of respiratory rhythm
respiratory center
spinal cord
Motor neurons that innervate respiratory muscles, their cell bodies are located in the anterior horn of the spinal cord in cervical segments 3 to 5 (which innervates the diaphragm) and thoracic segments (which innervate the intercostal muscles and abdominal muscles)
Respiratory neurons in the spinal cord are relay stations that connect high-level respiratory centers and respiratory muscles, and integrate the primary centers of certain respiratory reflexes.
lower brainstem
pons
upper part
Respiratory adjustment center (PC)
Inhibitory effect on the long-inhalation center
lower part
long suction center
Produces tonic facilitation on inhalation activity, prolonging inhalation
The vagus nerve can also promote the conversion of inhalation into exhalation. When the lower part of the pons loses the inhibition from the upper part of the pons and the promotion effect of the vagus nerve, inhalation cannot be converted into exhalation in time, which is manifested as long inhalation breathing.
Medulla oblongata
wheezing center
Irregular breathing movements can produce the most basic breathing rhythm
Medulla oblongata is the basic respiratory center
The respiratory rhythm bar is mainly generated in the premedulla Bauchinger complex.
Respiratory neurons (rhythmic spontaneous firing and rhythm related to the respiratory cycle)
Dorsal respiratory group (DRG) dorsomedial to medulla oblongata
Excites the phrenic motor neurons of the spinal cord, causing the diaphragm to contract and inhale
Ventral respiratory group (VRG) in the ventrolateral medulla
Calm breathing has no obvious effect
The body's metabolism is strengthened, and the respiratory motor neurons of the spinal cord are excited, which strengthens inhalation, triggers active exhalation, and increases pulmonary ventilation.
Pontine Respiratory Group (PRG) dorsal to the rostral pons
Restrict inhalation and promote the transition from inhalation to exhalation
Biot breathing
Performance
After one or more strong breaths, there is a prolonged respiratory arrest, followed by several strong breaths again, with a period of 10 seconds to 1 minute.
visible in
Brain injury, increased cerebrospinal fluid pressure, meningitis
significance
Critical symptoms that precede death
reason
The disease has invaded the respiratory center of the medulla oblongata
higher brain
Hypothalamus, limbic system, cerebral cortex, etc.
Respiratory movement is dually regulated by the voluntary nature of the cerebral cortex and the autonomy of the lower brainstem
Separation of spontaneous breathing and voluntary breathing
Autonomous rhythmic breathing is abnormal or even stops, and you can breathe at will
visible in
Damage to the spontaneous respiratory pathway descending from the anterolateral cord of the spinal cord
significance
Once the patient falls asleep, breathing stops and requires an artificial ventilator to maintain lung ventilation.
Able to breathe independently, unable to control breathing movements at will
visible in
Damage to motor areas of cerebral cortex or corticospinal tract
The mechanism of respiratory rhythm
pacemaker cell theory
neuron network theory
reflex regulation of breathing
chemoreceptive respiratory reflex
Chemical factors refer to CO₂, O₂, H in arterial blood, tissue fluid, and cerebrospinal fluid
chemoreceptors
peripheral chemoreceptors
carotid body and aortic body
Arterial blood PO₂, PCO₂ or H concentration increases → peripheral chemoreceptors are stimulated → along the sinus nerves (carotid body) and vagus nerve (aortic body) → nucleus of the solitary tract of the medulla → reflexively causes breathing to deepen and accelerate
The carotid body mainly regulates respiration, and the aortic body mainly regulates circulation.
Sensitive to a decrease in PO₂, but insensitive to a decrease in O₂ content
Anemia or CO poisoning→Oxygen content decreased, PO₂ normal
Physiological function
Low O₂ in the body maintains the drive for breathing
central chemoreceptor
Medulla oblongata central chemosensitive area
Superficial part of ventrolateral medulla oblongata
physiological stimulation
H in cerebrospinal fluid and local extracellular fluid
Blood CO₂ quickly passes through the blood-brain barrier → the concentration of extracellular fluid H around the chemoreceptors increases → stimulates the central chemoreceptors → breathing deepens and accelerates, and pulmonary ventilation increases
Blood H cannot easily penetrate the blood-brain barrier, and pH has a weak stimulating effect on central chemoreceptors.
adaptation phenomenon
Performance
CO₂ continues to increase. In the first few hours, the respiratory excitement response is obvious, and then in 1-2 days, the respiratory excitement response weakens to 1/5.
CO₂ in the blood has a strong acute driving effect on respiratory movement and a weak chronic stimulation.
reason
Kidneys regulate blood pH
Blood HCO3- can slowly pass through the blood-brain barrier, weakening the stimulating effect of H on respiratory movements
Physiological function
Regulates cerebrospinal fluid H concentration by affecting pulmonary ventilation and maintains a stable pH in the central nervous system
Regulation of respiratory movement by CO₂, H and O₂
CO₂ levels
The most important physiological and chemical factors that regulate respiratory movements
A certain level of PCO₂ is necessary to maintain the basic activity of the respiratory center. Hyperventilation can inhibit respiratory movement due to increased CO₂ elimination.
Increased inspiratory CO₂ concentration/pulmonary ventilation disorder → PCO₂ rise → reflex breathing deepens and accelerates → CO₂ excretion increases, blood PCO₂ returns to normal level
CO₂anaesthesia
Blood PCO₂ is too high, suppressing CNS → dyspnea, headache, dizziness, coma
CO₂ stimulates breathing
central chemoreceptor
Arterial blood PCO₂ increases by 2mmHg, stimulating central chemoreceptors and enhancing pulmonary ventilation.
Main effect, slow response
peripheral chemoreceptors
Arterial blood PCO₂ increases by 10mmHg, stimulating peripheral chemoreceptors and enhancing pulmonary ventilation.
Rapid respiratory response plays an important role
Cheyne-Stokes
Performance
Respiratory movement increases and decreases alternately, with a cycle of 45s~3min
visible in
Heart failure or brainstem damage
mechanism
There is a time difference between alveolar air and chemoreceptor PCO₂ and the feedback gain is too strong
H concentration
Arterial blood H concentration increases, breathing deepens and accelerates, and pulmonary ventilation increases
Regulatory mechanism
central chemoreceptor
High sensitivity but slow acting
Peripheral chemoreceptors (primary)
O₂ level
The PO₂ of the inhaled air decreases, which reflexively causes the respiratory movement to deepen and accelerate (PO₂ does not manifest until the PO₂ drops to 80mmHg, so severe hypoxia is of great significance)
Regulatory mechanism
Severe emphysema, pulmonary heart disease → chronic O₂ deficiency, CO₂ retention → central chemoreceptors adapt to CO₂ stimulation → low O₂ becomes the main stimulating factor for peripheral chemoreceptor stimulation
Chronic pulmonary ventilation or pulmonary ventilation disorders can cause respiratory depression due to inhalation of pure oxygen to relieve the stimulation of hypoxia.
Interaction of CO₂, H, O₂ in the regulation of respiratory movement
They can be strengthened by mutual synergy or weakened by mutual cancellation.
pulmonary stretch reflex
lung expansion reflex
When the lungs expand, the stretch receptors are excited by stretching the respiratory tract, and the impulses increase. The impulses are transmitted to the medulla oblongata via the vagus nerve, and through the action of the medulla oblongata and the pontine respiratory center, the inhalation is converted into exhalation.
The vagus nerve is severed, reflexes disappear, inhalation cannot be converted into exhalation in time, inhalation is prolonged, and breathing becomes deeper and slower.
Calm breathing generally does not participate in regulation. Only when the tidal volume exceeds 1500ml can the lung expansion reflex be triggered.
Lung compliance decreases, lung expansion stimulates airway stretch, causing reflexes, and breathing becomes shallower and faster.
lung collapse reflex
Enhance inspiratory activity or promote the conversion of exhalation to inhalation when the lung is collapsed
defensive breathing reflex
cough reflex
The larynx, trachea, bronchi, and mucous membranes receive mechanical or chemical stimulation → the impulse is transmitted along the vagus nerve to the medulla oblongata → cough (clear respiratory secretions or foreign bodies)
sneeze reflex
Nasal mucosal receptors → trigeminal nerve afferent to medulla oblongata → sneeze (clear nasal cavity irritants)
Respiratory muscle proprioceptive reflex
Respiratory movement and its regulation under special conditions
Physiological parameters and significance of clinical monitoring of respiratory status
blood oxygen saturation
arterial blood gas analysis
Mechanical Ventilation